Sachin Tapasvi, Sachin Jain, Ashok Shyam
Volume 1 | Issue 1 | April – Jun 2016 | Page 11-15
Author: Sachin Tapasvi [1 ], Sachin Jain [2], Ashok Shyam [2],[3]
[1] Orthopaedic Specialty Clinic, Pune, Maharashtra. India
[2] Sancheti Institute for Orthopaedics & Rehabilitation, Pune, India
[3] Indian Orthopaedic Research Group, Thane, India
Address of Correspondence
Dr Sachin Tapasvi
Orthopaedic Specialty Clinic, Pune Maharashtra. India.
Email: stapasvi@gmail.com
Abstract
Bone patella tendon bone (BPTB) graft versus Hamstring (HT) Graft is still an issue that is debated. Both the graft have stood the test of time with high patient satisfaction however each have their own advantages and disadvantages. BPTB has advantages of good stability and bone to bone healing and disadvantage of anterior knee pain, numbness and quadriceps weakness. HT graft have advantage of less donor site morbidity, less extension deficit and disadvantage of having a slightly higher failure rate and hamstring weakness. Irrespective of these named advantages and disadvantages the patient reported outcomes are similar with both graft and difference in choice of graft is poorly understood. In this review we simply try to bring our reader up-to-date with the current literature on this controversy
Keywords: Bone patella tendon bone graft, hamstring graft, anterior cruciate ligament reconstruction.
Introduction
Anterior cruciate ligament (ACL) is required for static and dynamic stabiliser of the knee joint and purpose of ACL reconstruction is to stabilize and to resume function to maximum extent (1, 2). The ideal graft for use in anterior cruciate ligament reconstruction should have structural and biomechanical properties similar to those of the native ligament, permit secure fixation and rapid biologic incorporation, and limit donor site morbidity (3). Moreover, these properties should be present at the time of graft implantation and persist throughout the incorporation period too (3).
Graft options available are broadly grouped into autograft such as bone patellar bone tendon graft (BPTB), hamstring graft, Quadriceps graft and allograft such quadriceps, patellar, Achilles, hamstring, and anterior and posterior tibialis tendon graft (3-6). Allografts are useful to minimize donor site morbidity but are associated with increased cost, slower incorporation time, increased risk of disease transmission, and a higher failure rate (2). The synthetic grafts are yet to prove themselves and currently the most commonly used graft used for ACL reconstruction are autografts namely hamstring or BPTB graft. With BPTB graft comes with advantages of excellent initial fixation, biomechanical properties, durability, success at long- term follow-up with reduced pivot shift test (7, 8) and disadvantage of few reports suggesting donor site morbidity of patellofemoral osteoarthritis, scar formation with shortening of the patellar tendon, loss of terminal knee extension, and patellofemoral pain(2,9,10).
Semitendinosus and gracilis tendons (quadrupled hamstring tendon [HT]) have found to minimize donor site morbidity causing less anterior pain(8) with disadvantage of numbness of the anterior knee caused by injury to the infrapatellar branch of the saphenous nerve during graft harvest(2), longer rehabilitation period(3,10) and persisting pivot shift test at long term follow up(7). There are multiple extrinsic and intrinsic confounding variables(11) while studying the results of ACL reconstruction out of which isolated effects of a single extrinsic variable of graft choice is to be made.
Method of Review
There are several review articles published in literature including Pubmed, Medline and Cochrane database to compare of graft superiority (hamstring versus BPTB) in ACL reconstruction. We primarily did a pubmed search with Bone-Patellar Tendon-Bone Grafting as the Mesh major keyword. Two hundred and eighty five article were found and reviewed. There were 51 articles that either compared the two grafts or were meta-analysis of such articles. These 51 articles were then further reviewed to construct this review. There were 9 metanalysis among these 51 articles and 3 additional systematic reviews (1,4,7, 11-20). The Cochrane review of 2011 and a systematic summary of systematic reviews was also added to this list (21,22). Results of all these reviews were compiled and presented in Table 1. Other relevant articles were added to the review depending on the significance of their findings. It was noted that in most article the main areas of comparison between the two grafts were stability, donor site morbidity, complications, rehabilitation status, functional outcomes and revision rates due to graft. The present review is also arranged in this format.
Functional outcome
Functional outcome was measured in most of the articles using scores like Lysholm knee score, Tegner activity level, International Knee Documentation Committee (IKDC) scores etc. None of the studies found any difference in functional outcome measured (1,4,7,11-19,23-25) and hence both the grafts are equally effective in terms of restoring the functional ability of the patients. Pinczewski et al noted that Level 1 and 2 sports activities were significantly reduced from 73 to 85% (short term) to 45-57% (long term results) in both HT and BTPB groups (11). Recent review mentions that patients with HT graft are almost twice more likely to return to sports but patient with BPTB Graft are more likely to return or exceed the preoperative sports level (22). Other also indicate that patients with BPTB graft return to activity earlier than the HT graft (12). This may be probably because BPTB graft provide more static and rotational stability (1,15). Poolman et al (17) commented that modern techniques of HT graft will further increase stability and improve return to activity. However this is not confirmed by recent articles and possibly better controlled trials will be needed to eventually answer the question.
Donor site morbidity and complication after graft harvesting
When overall incidence of morbidity was reviewed, HT graft patient have lower incidence of morbidity (12,15). Anterior knee pain and kneeling pain was significant in BTPB group as compared with HT group(1–3,11,23). Anterior knee pain is related to the secondary chondromalacia patella which happens after ACL reconstruction regardless of graft type but it is noted that it can be five times greater in BPTB group versus HT group(2). There was a significant extension loss of >5 degrees in BPTB group versus HT group(1). It is noted that there was a concentric and eccentric reduction in Quadriceps power which was related to poor satisfaction rates (23). The Cochrane review in 2011 noted that BPTB Graft resulted in loss of knee extension range and strength while HT graft showed trend toward loss of flexion range and strength (21). There was a slight risk of patellar fracture which was mainly related to the errors in the surgical technique or use of unnecessary deeper saw cuts or osteotomes(23). Other donor site problems noted are patellar tendinitis, rupture of patellar tendon, increased joint stiffness, late chondromalacia and injury to infrapatellar branch of saphenous nerve(2,3,23). Reduced ultimate range of motion may be related to the rigid construct used in fixing BPTB graft (2). Other disadvantage of hamstring graft are injury to the superficial branch saphenous nerve and weakness of the hamstring muscles after operation (23, 24).
Stability
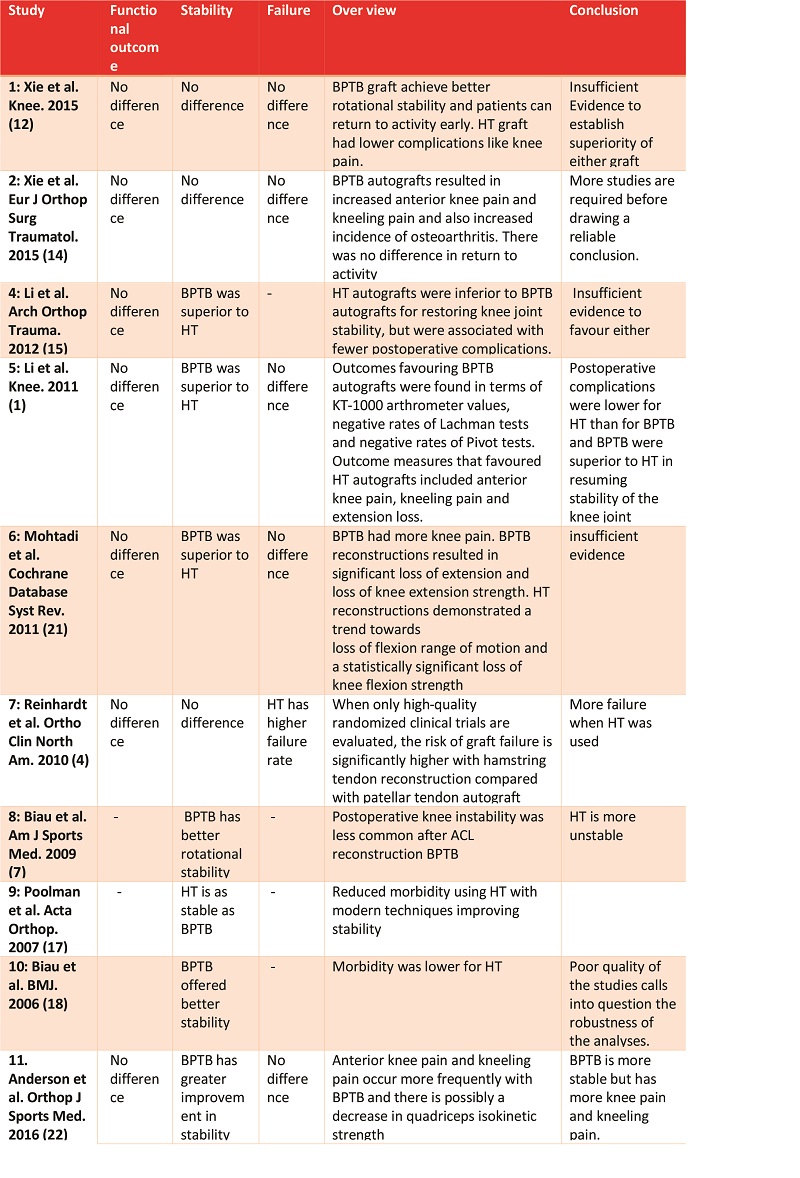
Stability has shown varied results in different studies and possible is a function of surgical technique and rehabilitation [Table 1].
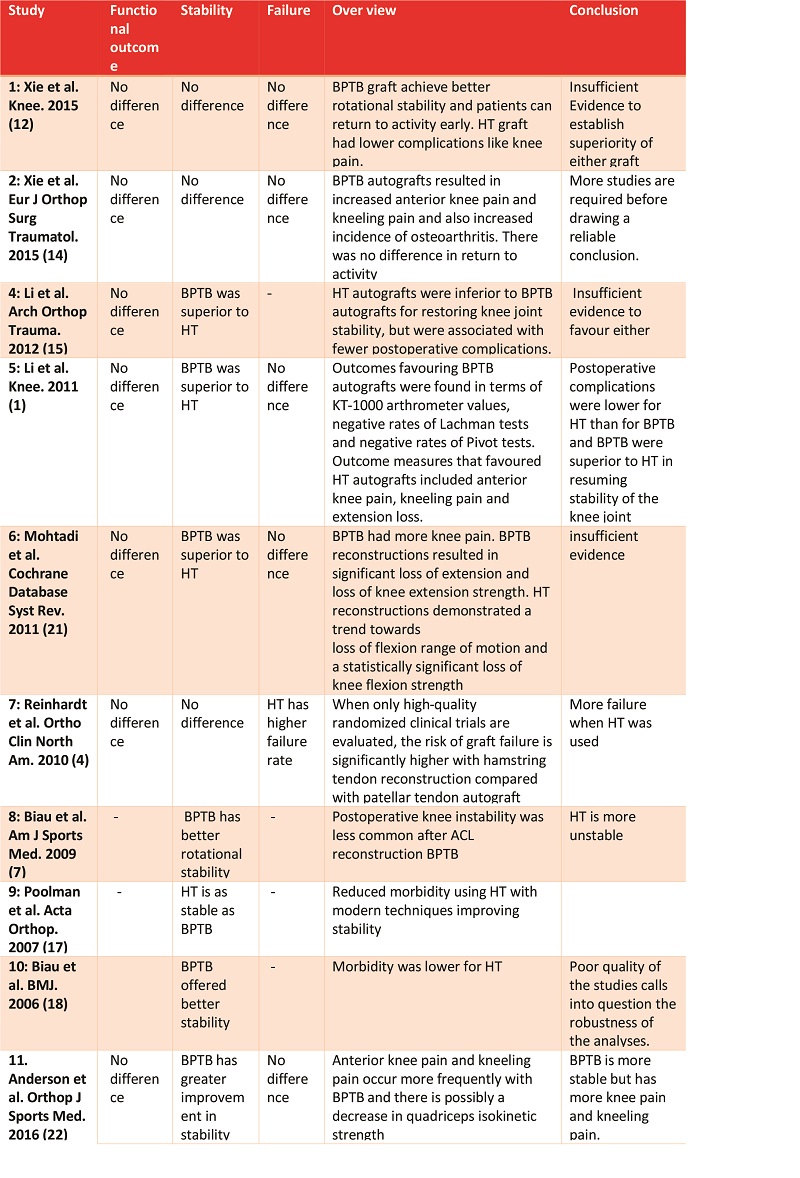
Table 1: Comparative analysis of meta-analysis comparing BPTB and HT autograft
Stability was assessed by Lachman test, pivot shift test and KT -1000 arthrometer in most series. Some authors reported no significant difference between either HT or BPTB group at long term follow up (11, 2). However, in mid-term follow up the side-to-side instrumented laxity (>2 mm) was greater in HT group as compared to BPTB group (7). BTPB is also found to be more rotationally stable with respect to pivot shift test (1).
Stability in case of HT graft was based on the number of strands used during surgery when compared with BPTB graft (1). When a 2 strand HT graft was used a statistical difference was noted in case of KT – 1000 and pivot shift test in favour of BPTB graft whereas Lachman test was not significant in both groups. If a 4 strand HT graft with a suspensory fixation like endobutton was used then the statistical difference was not significant in both the groups and had near normal Lachman, pivot shift tests and KT – 1000 testing(1,10,26–28). There is a slightly higher degrees of laxity noted in quadrupled hamstring graft as compared with BPTB graft especially in females in long term studies(2,20). Cochrane review noted that BPTB reconstructions are more likely to result in statically stable knees but they are also associated with more anterior knee problems. However there is insufficient evidence to predict superiority of one graft over other in long results in respect to functional outcome(21). In a study, comparing double bundle reconstruction with HT graft and anatomical BPTB graft positioning equal results are found with respect to stability and laxity throughout the range of motion(29). The recent summary of meta-analysis however concluded that BPTB graft are more stable as per the current available evidence (22)
Rehabilitation
It is noted that integration of bone to bone healing with direct insertion is much faster in BPTB graft as compared to bone to soft tissue healing by means of indirect insertions with sharpey’s fibres in case of HT graft(23). So with rapid incorporation with graft healing to bone, there is potential for accelerated rehabilitation in BPTB graft and may be earlier return to play sports activities(3,23). It usually takes 6 weeks for a BPTB to incorporate in the host bone whereas around 8 to 12 weeks with HT graft(3). Short term studies showed mixed results of quadriceps strength with HT graft harvest whereas long term studies shows no difference in quadriceps strength with BPTB versus HT graft(8,20). Evaluation of functional capacities: power, strength, velocity and dynamic stability of knee extensor and flexor muscles after ACL reconstruction showed that use of a BPTB autograft achieved better muscular and functional capacities than the HT autograft(6). During rehabilitation with hamstring graft requires less supervision with less risk of complications such as the infrapatellar contracture syndrome, arthrofibrosis or persisting pain(23).
Osteoarthritis Risk
Radiographic assessment showed no significant differences between the two groups in terms of osteoarthritic findings classified according to the Fairbank and Ahlback rating systems in short term studies(26) and mild osteoarthritic changes in BPTB group at mid and long term follow up as compared with HT group(11). Overall, osteoarthritis was identified in 16% (BPTB 19%; ST 13%.) according to the Ahlback rating system and 68% (BPTB 67%; ST 70%; ) according to the Fairbank rating system(26). Xie et al found the risk of development of OA was around 61% greater in BPTB graft as compared to HT Graft (14). Early osteoarthritic changes are also function of primary injury and associated injuries like meniscal injuries and cartilage injuries (30). However late onset osteoarthritis will require much longer follow up and none of the current studies offer much insight into development of OA in long term (22)
Failure rates
There is no obvious difference in the occurrence of ligament failure between HT group and the BPTB group after ACL reconstruction in long term studies but a few studies demonstrate reduced failure rates with BPTB graft(1). Hamstring graft harvest weakens the knee flexor strength leading to slightly higher degrees of graft failure (2,4). However, these studies had a selection bias which had included studies using double or triple strand graft which gave slightly higher failure rates. Long term studies have shown to have equal success rates with quadrupled hamstring graft or BPTB graft(8,20). Moreover, it is also noted that the fixation modality and anatomical placement of ACL is responsible for low failure rates(20) It has been noted that contralateral ACL tear with BPTB graft is statistically significant as compared to HT graft in short term studies whereas in long term studies there is no increase in contralateral ACL tear(8). A risk factor for contralateral ACL rupture was a return to sports that involved sidestepping, pivoting, and jumping (8). In a registry study based on 45,998 primary ACL Reconstructions in Scandinavi it was found that patients receiving patellar tendon autografts have a statistically significantly lower risk of revision compared with patients receiving hamstring autografts(5).
Conclusions
As per current reviews and evidence, both graft achieve good functional outcome in patients. BPTB graft may offer a more stable knee and possible achieve rapid and effective return to preinjury activity level. HT graft have less donor site morbidity and with new effective fixation modalities, they may also match the stability achieved by BPTB grafts. However there is insufficient evidence to clearly establish a winner and probably more robust future studies will be better able to define the role of each of these autograft options
References
1. Li S, Su W, Zhao J, Xu Y, Bo Z, Ding X, et al. Review A meta-analysis of hamstring autografts versus bone – patellar tendon – bone autografts for reconstruction of the anterior cruciate ligament. Knee 2011;18(5):287–93.
2. Shelton WR, Fagan BC. Autografts Commonly Used in Anterior Cruciate Ligament. J Am Acad Orthop Surg. 2011;19(5):259–64.
3. West R V, Harner CD. Graft Selection in Anterior Cruciate Ligament Reconstruction. J Am Acad Orthop Surg. 2005;13(3):197–207.
4. Reinhardt KR, Hetsroni I. Graft Selection for Anterior Cruciate Ligament Reconstruction : A Level I Systematic Review Comparing Failure Rates and Functional Outcomes. Orthop Clin NA [Internet]. Elsevier Ltd; 2010;41(2):249–62.
5. Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G. Lower Risk of Revision With Patellar Tendon Autografts Compared With Hamstring Autografts A Registry Study Based on 45 , 998 Primary ACL Reconstructions in Scandinavia. Am J Sports Med. 2014;42(10):2319–28.
6. Baur C, Mathieu N, Delamorclaz S, Hilfiker R, Blatter S, Siegrist O, et al. Anterior cruciate ligament reconstruction : Hamstring Tendon autograft versus Bone Patellar Tendon Bone autograft : what about muscular and functional capacities ? Schweizerische Zeitschrift für Sport und Sport. 2015;63(2):18–22.
7. Biau DJ, Katsahian S, Kartus J, Harilainen A, Feller JA, Sajovic M, et al. Patellar Tendon Versus Hamstring Tendon Autografts for Reconstructing the Anterior Cruciate Ligament : A Meta-Analysis Based on Individual Patient Data. Am J Sports Med. 2009;37(12):2470–8.
8. Macaulay AA, Perfetti DC, Levine WN, Macaulay AA, Perfetti DC, Levine WN. Anterior Cruciate Ligament Graft Choices. Sport Heal A Multidiscip Approach. 2012;4(1).
9. Dahm DL. A Meta-analysis of Patellar Tendon Autograft Versus Patellar Tendon Allograft in Anterior Cruciate Ligament Reconstruction. Arthrosc J Arthrosc Relat Surg. 2008;24(3):292–8.
10. Siebold R, Webster ÆKE, Feller ÆJA, Sutherland AG, Elliott ÆJ. Anterior cruciate ligament reconstruction in females : a comparison of hamstring tendon and patellar tendon autografts. Knee. 2006;14:1070–6.
11. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-Year Comparison of Anterior Cruciate Ligament Reconstructions With Hamstring Tendon and Patellar Tendon Autograft A Controlled , Prospective Trial. Am J Sports Med. 2007;10(10):1–11.
12. Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015 Mar;22(2):100-10
13: Yao LW, Wang Q, Zhang L, Zhang C, Zhang B, Zhang YJ, Feng SQ. Patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2015 Feb;25(2):355-65.
14. Xie X, Xiao Z, Li Q, Zhu B, Chen J, Chen H, Yang F, Chen Y, Lai Q, Liu X. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol. 2015 Jan;25(1):149-59.
15. Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg. 2012 Sep;132(9):1287-97
16. Biau DJ, Katsahian S, Nizard R. Hamstring tendon autograft better than bone-patellar tendon-bone autograft in ACL reconstruction – a cumulative meta-analysis and clinically relevant sensitivity analysis applied to a previously published analysis. Acta Orthop. 2007 Oct;78(5):705-7
17. Poolman RW, Farrokhyar F, Bhandari M. Hamstring tendon autograft better than bone patellar-tendon bone autograft in ACL reconstruction: a cumulative meta-analysis and clinically relevant sensitivity analysis applied to a previously published analysis. Acta Orthop. 2007 Jun;78(3):350-4.
18. Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006 Apr 29;332(7548):995-1001.
19. Harilainen A, Linko E, Sandelin J. Randomized prospective study of ACL reconstruction with interference screw fixation in patellar tendon autografts versus femoral metal plate suspension and tibial post fixation in hamstring tendon autografts: 5-year clinical and radiological follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006 Jun;14(6):517-28.
20. Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004 Dec;32(8):1986-95.
21. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011 Sep 7;(9):CD005960.
22. Anderson MJ, Browning WM 3rd, Urband CE, Kluczynski MA, Bisson LJ. A Systematic Summary of Systematic Reviews on the Topic of the Anterior Cruciate Ligament. Orthop J Sports Med. 2016 Mar 15;4(3):2325967116634074.
23. Bartlett RJ, Clatworthy MG, Nguyen TN V. Review article GRAFT SELECTION IN RECONSTRUCTION OF THE ANTERIOR CRUCIATE LIGAMENT. J Bone Joint Surg Br. 2001;83(July):625–34.
24. Matjaz S, Andrej S, Radko K, Mojca D. The effect of graft choice on functional outcome in anterior cruciate ligament reconstruction. Int Orthop. 2008;32:473–8.
25. Martin NJ, Shishir SM, Kanagasabai R, Najimudeen S, Gnanadoss JJ. “ Quadruple hamstring tendon graft versus Bone-Patellar- Tendon-Graft for arthroscopic Anterior Cruciate Ligament reconstruction- comparison study with follow up of 2 years .” IOSR J Dent Med Sci. 2014;13(11):6–13.
26. Ahlde M. Knee laxity measurements after anterior cruciate ligament reconstruction , using either bone – patellar – tendon – bone or hamstring tendon autografts , with special emphasis on comparison over time. Knee. 2009;17:1117–24.
27. Svensson M, Ejerhed L, Kartus T. A prospective comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction in female patients. Knee Surgery, Sport Traumatol Arthrosc. 2006;14:278–86.
28. Gauti L, Ninni S, Lars E, Jon K, Juri K. A prospective comparison of bone-patellar tendon-bone and hamstring tendon grafts for anterior cruciate ligament reconstruction in male patients. Knee. 2007;15:115–25.
29. Ishibashi Y, Tsuda E, Fukuda A, Tsukada H. Intraoperative Biomechanical Evaluation of Anatomic Anterior Cruciate Ligament Reconstruction Using a Navigation System Comparison of Hamstring Tendon and Bone – Patellar Tendon – Bone Graft. Am J Sports Med. 2008;36(10):1903–12.
30. Andersson D, Samuelsson K, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: an assessment of randomized controlled trials. Arthroscopy. 2009 Jun;25(6):653-85
| How to Cite this article:. Tapasvi S, Jain S, Shyam AK. BTB Vs Hamsrtings – Is There a Winner Yet ?. Asian Journal of Arthroscopy Apr-June 2016;1(1):11-15 . |
 Dr. Sachin Tapasvi |
 Dr. Sachin Jain |
 Dr. Ashok Shyam |