Jonathan Herald, Sagar Kakatkar
Volume 1 | Issue 1 | April – Jun 2016 | Page 16-19
Author: Jonathan Herald [1], Sagar Kakatkar [1]
[1] Orthoclinic, Sydney, Australia.
[2] Dr. Vasantrao Pawar Medical College and Hospital, Nashik, India.
Address of Correspondence
Dr. Sagar Kakatkar
Orthoclinic Sydney, Suite 1606, Level 16, 109 Pitt Street
Sydney NSW 2000 Sydney, Australia
Abstract
Immediate post-operative knee stability and early return to pre-injury activities are two goals of ACL reconstruction today. Autografts and Allografts when used for the ACL reconstruction are based on a principle of graft incorporation in the tunnels which renders them inefficient in providing immediate stability after the surgery. Since post-operative rehabilitation protocols after allograft or autograft ACL reconstruction are designed to protect the grafts for a certain period, early return to pre-injury functional status is not possible. Apart from these disadvantages, graft related complications and availability of the grafts are problems for both autografts and allografts. Synthetic ACL substitutes have been developed, modified and re-modified according to the clinical outcomes and reported complications. And although few of them have shown early promising results, whether they can stand the test of time or not is still to be seen.
Key words: Anterior cruciate Ligament (ACL), Ligament Advanced Reinforcement System (LARS), Synthetic grafts, Tissue engineering, Leeds-Keio artificial ligament, ligament augmentation device(LAD)
Introduction
Improving the quality of life has been the principle focus of modern health care. Correspondingly, evaluation criteria for surgical outcomes have also changed. Achieving post-operative stability is no longer the only goal after ACL reconstruction; but ‘Early’ and ‘Sustained’ return to pre injury levels of activities is now considered as the measuring tool for success. ACL injury is the most common knee ligamentous injury in sports related activities and a delay in returning to sports is enough to ruin a sportsman’s career. Autografts and Allografts have been the main graft choices for ACL reconstruction. Autografts have shortcomings such as inadequate graft length or diameter and donor site morbidity while; allografts on the other hand have problems of allogenicity, insufficient supply of grafts, high costs, etc. A common disadvantage that both these grafts share is the requirement of integration of the graft in the osseous tunnels. Time required for this integration process is variable and subjective and is more for allografts than autografts (14).
Extensive research has been done to overcome these problems associated with autografts and allografts and to develop a suitable synthetic substitute for ACL reconstruction. But since 1918 when Alwyn- Smith tried ACL reconstruction with silk sutures for the first time, use of synthetic grafts for the ACL reconstruction has been a tale of failures(16).
Expectations from Synthetic grafts and the their Evolution
Synthetic graft technology has evolved from non-biological to biological grafts. The grafts are developed so as to have better strength compared to native ACL. Their use is designed to reduce not only the donor site morbidity but surgical time also. The greatest function which they are supposed to serve is to provide immediate post-operative stability to the knee thus promoting early mobilization, faster rehabilitation and quicker return to pre injury level activities.
The synthetic replacements that have been used for the ACL can be broadly classified into three types which also follows their chronological order(16).
Class 1: Graft Fibers:
These include fibers of polyethylene, PTFE (Polytetrafluoroethylene). These were one of the few earlier graft substitutes and had high failure rates because of graft breakage.
Class 2: Ligament Augmentation devices (LAD):
These include polypropylene polyesters which were strong. These devices were used along with ACL autografts or allografts and were supposed to provide immediate structural support to the grafts so that to enhance their integration. But unfortunately these augments caused ‘stress shielding’ and led to delayed graft integration thus leading to higher incidences of graft failures.
Class 3: Prosthetic materials:
The earlier generations of these prostheses did not allow any soft tissue ingrowth and thus although they had good early functional results, the long term follow ups reported high failure rates. Second generation prostheses developed were based on the principles of combining structural properties of prosthetic material with tissue engineering to develop scaffolds for ACL reconstruction. These were supposed to provide good initial strength and then allow gradual soft tissue ingrowth for longevity. Following are the different types of prosthetic materials used clinically:
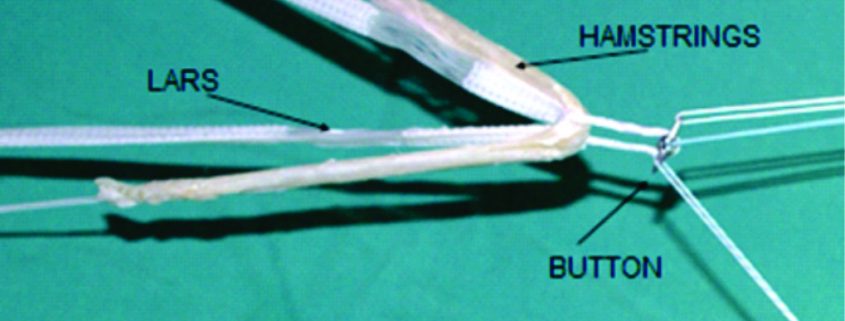
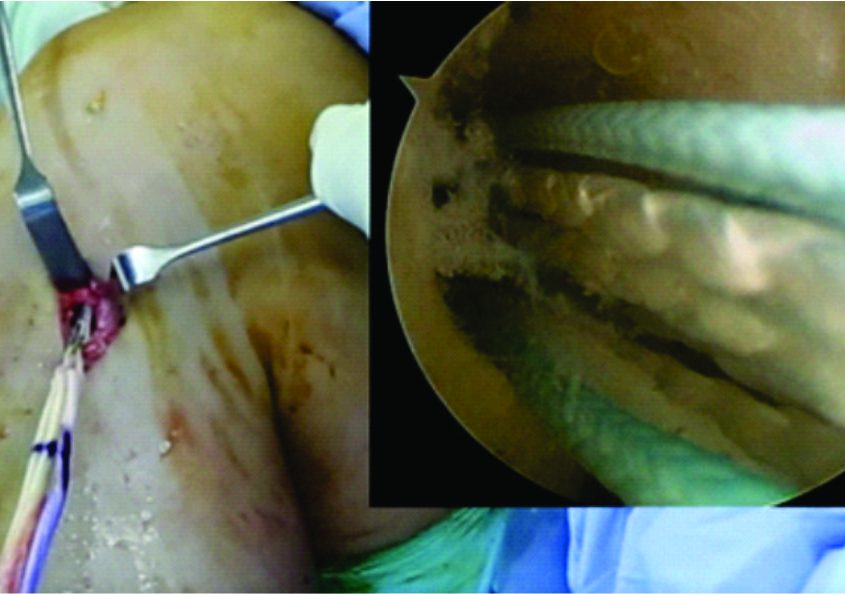
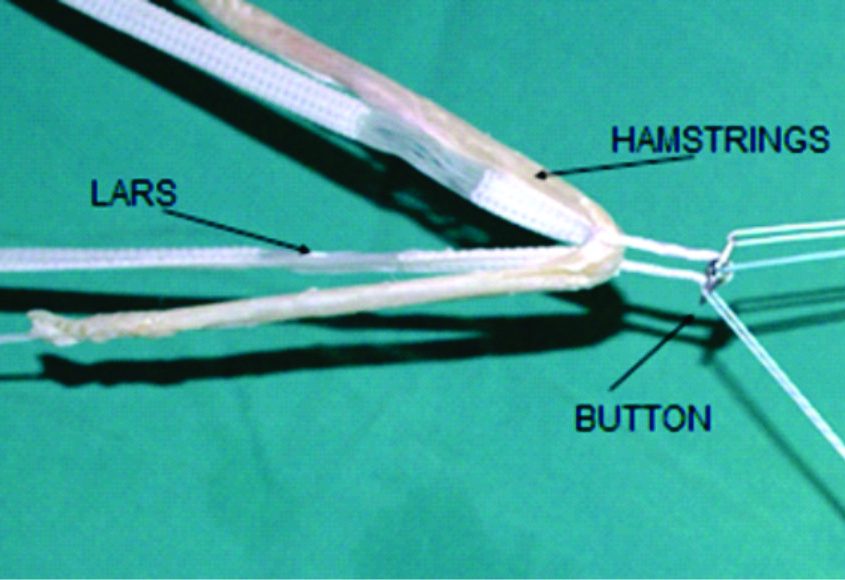
Figure 1 & 2: Show how the graft passage for the LARS should be sequential and gradual so as to correctly position the intraarticular and intraosseous parts of the LARS in their proper positions.
a) Carbon based prosthetic devices: These allowed collagen ingrowth but histopathological studies of the tissues tested showed accumulation of carbon particles in the lymphatic system of the individuals. Also these had high incidences of graft ruptures, disintegration and failures, so were discontinued.
b) Gore-Tex: These were probably the strongest synthetic graft substitutes which included expanded Polytetrafluoroethylene fiber looped on itself. Their use in ACL reconstruction had good functional outcomes and hence gained the FDA approval for use in patients with failed autologous intraarticular graft procedures i.e. for revision cases. However long term follow up showed increased incidences of loosening of the grafts which led to detrimental functional outcomes.
c) Leeds- Keio Artificial Ligament: Was developed by Fujikawa and Seedhom. This was one of the most popular synthetic substitute for the ACL reconstruction because of good early functional outcomes. The ligament was composed of a polyester mesh with tibial and femoral bone plugs attached for anchorage in the tunnels. It provided good soft tissue ingrowth and had good shear resistance. But because of its high tensile strength it acted as mainly a load bearing prosthesis and had poor long term results. There were many clinical studies reporting long term graft failures (8).
d) Kennedy ligament augmentation device (LAD): The good clinical results of LAD as reported by its developers were non reproducible and this synthetic substitute led to post-operative synovitis due to its Polypropylene structural units. The implant graft interface when used as an augmentation device was the weakest area of the construct and thus had graft failures.
A Landmark study done by Marie –France Guidoin, et al.(13) reported causes of failures in 117 synthetic ligamentous prosthesis which had failed either because of the rupture or recurrent synovitis. The type of prostheses excised include Gore-Tex, Kennedy LAD, PET based prostheses, etc. These prostheses were tested under scanning electron microscope (SEM) and following three mechanisms involved in the failure of these ACL prostheses were noted. 1) Failure because of inadequate fiber abrasion resistance against osseous structure 2) Flexural and rotational fatigue of the fibers 3) Loss of integrity of the textile structure due to tissue infiltration during healing. The second and third mechanism of failure were the most difficult problems to address.
e) LARS (Ligament Advanced reinforcement system): This is the latest development in the synthetic ligament substitutes. It consists of polyethylene tetraphthalate (PET) as the structural component. The LARS has been designed to mimic ligamentous anatomy. It has 2 parts i.e. intra articular and intraosseous part. The intraosseous part is composed of longitudinal fibers of PET held together with transverse knitted structure. While the intraarticular part has parallel longitudinal fibers of PET twisted perpendicular to each other. These parts should be aligned perfectly while doing the ACL reconstruction to avoid early graft failures (Figure 3). The orientation of the fibers is modified to be side specific i.e. different for left and right knees thus mimicking the 3D cross-sectional anatomy of intraarticular part the native ACL. This is supposed to help overcome rotational fatigue of the synthetic ligament. Although this is a far superior structural construct compared to other synthetic substitutes, getting the LARS intraosseous part and intraarticular part exactly in their place during the surgery requires excellent surgical skill (Figure 1 and 2). The LARS also promotes tissue ingrowth(17).
|
Several studies considering the outcomes following LARS for the ligamentous reconstruction showed good to excellent functional outcomes and good patient satisfaction (4, 7, 9, 10, 12, 15). A few of the papers even rated LARS as better than the autograft ACL reconstructions (9,6, 18). Histopathological studies do support the cellular ingrowth with LARS acting as a scaffold (17).
If return to pre injury level is considered as the criteria for success, few studies report LARS enabling patients to go back to active sports related activities within 2-3 months of the surgery (19). But the study done by Zuzana Makotka et al. in 2010 which was a meta-analysis of the literature published on LARS for ACL reconstruction from year 2000 to 2010 showed that none of the studies done on LARS autologous ‘ligamentous’ healing along the synthetic meshwork of LARS. Even though LARS is thought to reduce the surgical time, none of the studies had commented about the duration of surgery with the LARS ACL reconstruction. None of the study compared return to previous level of function with LARS and with traditional ACL reconstruction. This metaanalysis was based on the 4 studies and also stated that LARS may not be good for chronic ACL injuries as in such cases quality of remnant of the ACL i.e. ACL stump is not good and LARS may not have good ligamentous ingrowth on fibrotic stump.
Considering the latest literature, Alberto et al. in their study published in 2014 showed that a few patients with failed reconstruction with Polyethylene tetraphthalate (PET) synthetic grafts (1). Fourteen of such patients underwent revision surgery performed as two-staged revision. All these patients has histopathological evidence of granulomatous reaction due to PET. And even the revision surgeries done with the autografts did not improve functional status of these patients or stop the progressive Osteoarthritis occurring in these patients. In another study the rate of failure of LARS in a 19 year outcome study was reported to be 27.5% with 100% patients presenting with degenerative arthritis (2).A few other studies report disabling synovitis secondary to LARS ACL reconstructions (5).
Hence till date, the literature regarding the LARS remains controversial and there are no studies comparing early on long term outcomes of the LARS and those with autograft/ Allograft ACL reconstructions.
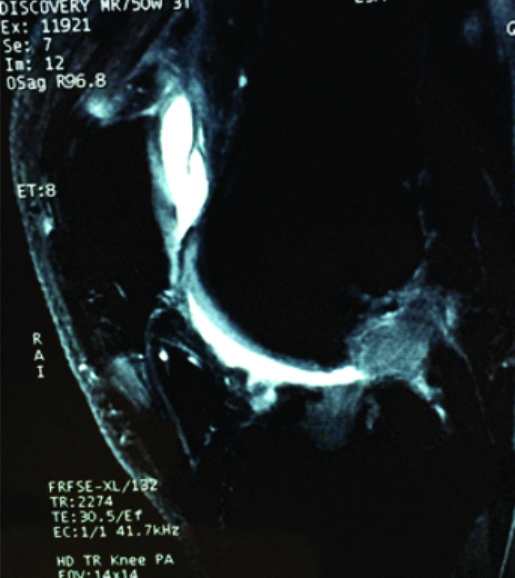
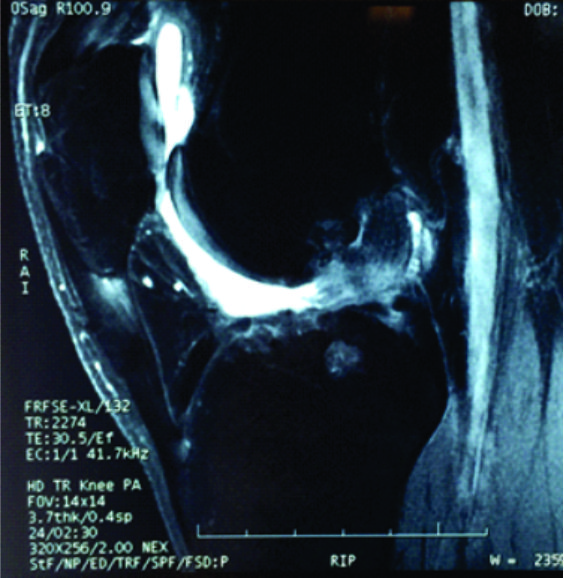
In authors practice, several cases treated by LARS ACL reconstruction elsewhere, which are symptomatic either because of graft loosening or graft failure have been encountered(Figure 4,5,6). Of those patients who underwent revision surgeries, histopathological examination of the synovial tissue collected during surgery showed chronic granulomatous inflammation and the patients, in spite of attaining knee stability continued to have symptoms due to inflammatory synovitis and progression of arthritis. When tested using new battery of tests which used to evaluate return to sports status of the patients with ACL reconstruction; patient’s ability to return to sports related activities was better in patients treated with autograft ACL reconstruction than LARS ACL reconstruction and further evaluation of these patients is being done (4).
Apart from studies on LARS, latest literature which is a randomized study with or without synthetic degradable augmentation device to support autograft in ACL reconstruction, no significant difference in clinical outcomes in short, intermediate and long term prospective was found in between the two groups i.e. one group with the use of poly (urethane urea) augmentation device and other without it (11).
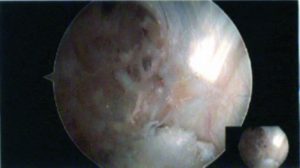
Figure 6: Arthroscopic picture of ruptured LARS stump with visible particulate debris of the LARS visible on the background of PCL
Future Prospects
Development of ideal synthetic scaffold for the ACL reconstruction is a difficult task to achieve. Efforts are in place to create a synthetic substitute which can provide immediate functional stability and which can degrade at a rate similar to that of the tissue ingrowth. With advancements in tissue engineering, several polymers with a variety of different cell types have been developed for the scaffolds. Since the Fibroblast added collagen scaffolds had problems of immunogenicity and variable physical properties, biodegradable polymers such as Polyglycolic acid scaffolds have been developed and have been tested on animal models. Several studies using bone marrow stromal cells for formation of fibroblasts and smooth muscle cells with slow degrading properties of the scaffolds have been done (16).
With constant improvements in the tissue engineering techniques, future seems to be bright for synthetic ligamentous substitutes but for now, we are yet to supersede the biological grafts for the ACL reconstruction.
References
1. Alberto Venturo, Claudio Legnani, Clara Terzaghi, Enrico Borgo, Walter Albisetti “Revision surgery after failed ACL reconstruction with artificial ligament: Clinical, Histological and Radiographic Evaluation’. Eur Journal Orthop Surgery Traumatol 2014 24:93-98.
2. Alberto Venturo, Claudio Legnani, Clara Terzaghi, Enrico Borgo, Walter Albisetti “Synthetic graft for anterior cruciate ligament rupture 19 year outcome study” The Knee 17 (2010) 108–113.
3. Caroline Hildebrandt, Lisa Muller, Barbara Zisch, Reinhard Huber, Christian Flink, Christian Raschner “ Functional Assessment for decision making regarding return to sports following ACL reconstruction Part 1: development of new test battery. Knee Surg Sports Traumatol Arthrosc 2015 23: 1273-1281.
4. Cerulli, G. et al. (2007). ACL reconstruction using artificial ligaments: Five years follow-up. S.I.O.T, 33 (3suppl. 1), pp. 8238-8242.
5. Constantine M. Glezos, Alison Waller, Henry E. Bourke, Lucy J. Salmon and Leo A. Pinczewski “Disabling Synovitis Associated With LARS Artificial Ligament Use in Anterior Cruciate Ligament Reconstruction: A Case Report” Am J Sports Med 2012 40: 1167.
6. Fan, Q. et al. (2008) Comparison between four-strand semitendinosus tendon autograft and ligament advanced reinforcement system for anterior cruciate ligament reconstruction by arthroscopy. Chinese Journal of Reparative and Reconstructive Surgery 2008 June (6): 676-9 2008.
7. Huang Jian-ming et al (2010) cruciate ligament reconstruction using LARS artificial ligament under arthroscopy: 81 cases report. Chinese Medical Journal, 2010; 132(2):160-164.
8. Jan Riding, Lars Peterson “ Clinical experience with the Leeds-Keio Artificial Ligament in Anterior cruciate ligament reconstruction: A prospective 2 year follow-up study The American Journal of sports medicine Vole 23, no 3,1995.
9. Jiao Chen ,AquinoGU, Haiti Jiang, Winnie Zhang ,Xian Grong Yu “A comparison of acute and chronic anterior cruciate ligamentreconstruction using LARS artificial ligaments: a randomizedprospective study with a 5-year follow-up” Arch Northup Trauma Surge (2015) 135:95–102.
10. Kai Ago, M.D., Shay Chen, M.D., Ph.D., Lied Wang, M.D., Weiguo Zhang, M.D.,Yifan Kang, M.D., Qirong Dong, M.D., Haibin Zhou, M.D., and Linan Li, M.D. “Anterior Cruciate Ligament Reconstruction with LARS ArtificialLigament: A Multicenter Study With 3- to 5-Year Follow-up” Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 26, No 4 (April), 2010: pp 515-523.
11. Lars Peterson, Ulf Eklund, Bjorn Engstorm, Magnus Forssblad “ Long term results of a randomized study on ACL reconstruction with or without a synthetic degradable augmentation device to support autograft” KSSTA 2014,22: 2109-2120.
12. Lavoie, P. et al. (2000). Patient satisfaction needs as related to knee stability and objective findings after ACL reconstruction using LARS artificial ligament. The Knee, 7, pp. 157-163.
13. Marie-France Guidoin, Yves Marois, Jaques Bejui, Nicolas Poddevin, Robert Guidoin,et al. “ Analysis of retrieved polymer fibers based replacement” Biomaterials 21(2000), 2461-2474.
14. Meinolf Goertzen, M.D. PhD “Donor tissue choices in ACL revision” Sports Medicine and Arthroscopy review 5: 128-135,1997.
15. Papadopoulos, G. et al. (2005). Long – Term Results In The Treatment Of Acl Ruptures Using The LARS – Artificial Ligament. A.L.S. , Salzburg, June , 10-12 , 2005.
16. Saccomanni Bernardino “ ACL prosthesis- Any promise for future” Knee Surg Sports Traumatol Arthros 2010 18: 797-804.
17. Trieb, K. et al. (2004). In vivo and in vitro cellular ingrowth into a new generation of artificial ligament, Eur Surg Res. May-Jun;36(3):148-51.
18. Zhong-tang Liu & Xian-long Zhang & Yao Jiang & Bing-Fang Zeng “Four-strand hamstring tendon autograft versus LARSartificial ligament for anterior cruciateligament reconstruction” International Orthopaedics (SICOT) (2010) 34:45–49.
19. Zuzana Makotka, Ian Scarborough, Sarvana Kumar, Luke Parraton, et al. “Anterior cruciate ligament repairs with LARS: A systemic review. Sports Med Arthroscopy, Rehab, Therapy and technology 2010, 2: 29.
| How to Cite this article:. Herald J, Kakatkar S. Synthetic Grafts in Anterior Cruciate Ligament Reconstruction. Asian Journal of Arthroscopy Apr- June 2016;1(1):16-19 . |