Imaging of Meniscus Repair and Healing : A Review of Current Trends/ Literature
Anupama S Patil, Aparna H Chandorkar
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 23-27.
Author: Anupama S Patil[1], Aparna H Chandorkar[1]
[1] Star Imaging and Research Centre, Joshi Hospital Campus, Opposite Kamla Nehru Park, Erandwane, Pune, India. Pin Code- 411004.
Address of Correspondence
Dr Anupama S Patil
Star Imaging and Research Centre, Joshi Hospital Campus, Opposite Kamla Nehru Park, Erandwane, Pune, India. Pin Code- 411004.
Abstract
Considerable developments have occurred in meniscal surgery, with increasing usage of meniscal repair as the preferred modality of treatment for meniscal tears, in order to preserve the meniscal morphology and physiologic function and to delay osteoarthrosis . Second look arthroscopy is considered the gold standard in assessing meniscal healing. However, arthroscopy being an invasive procedure, there is a need for developing accurate modalities for imaging of the post –repair status of the meniscus as a viable alternative to arthroscopy. Magnetic resonance imaging (MRI) is a good non invasive imaging modality for evaluation of meniscal healing . However, persistence of signals within a repaired healed meniscus on conventional MRI makes accurate interpretation difficult. MR arthrography (MRA), which involves addition of intra-articular contrast, increases the sensitivity and specificity of differentiation between healed scar and possible non healed repair/retear. CT arthrography is another imaging technique which has been used for detection of retear; however it is limited in the degree of information it provides as compared to MRI/MRA. This review aims to discuss the different imaging techniques available for the evaluation of post repair meniscus and its healing and the advantages and disadvantages of the same.
Introduction
The meniscus is important for preserving a multitude of normal functions of the knee joint such as shock absorption, force transmission, stability maintenance and joint lubrication [1]. These critical functions of an intact meniscus make it important to preserve as much meniscal tissue as possible in patients with meniscal injury. Thus, meniscal repair [rather than menisectomy] has become the optimal treatment for meniscal tears, especially for vertical or oblique linear tears located in the vascular zone [2, 3]. The main diagnostic tools for assessment of meniscal repair and meniscal healing are clinical assessment, MRI/MR arthrography, CT arthrography and second look arthroscopy [2, 4-6]. Second look arthroscopy remains the gold standard in evaluating the healing status. However, because of its invasive nature and cost, MRI/MR arthrography and CT arthrography are emerging as fairly good alternatives to arthroscopy [7, 8]. Clinical assessment includes criteria such as medial joint line tenderness, joint swelling, locking, pain on extreme flexion and a positive McMurrays test. It is the simplest method of assessment of the patient, but it is highly dependent on the experience of the surgeon [9]. MRI is a non invasive method of assessing the meniscus. Evaluation of a post operative meniscus is a challenge as the diagnostic criteria for MR evaluation of tear in a repaired meniscus are different from those in a virgin meniscus [7, 10]. The presence of post-operative signals sometimes confound the reading of the MRI. Addition of intra-articular contrast further aids differentiation of scar tissue versus tear [3, 7, 10, and 11]. This narrative review aims to discuss the different imaging methods for evaluation of meniscus repair and healing and the advantages and disadvantages of the same.
Assessment of meniscal healing:
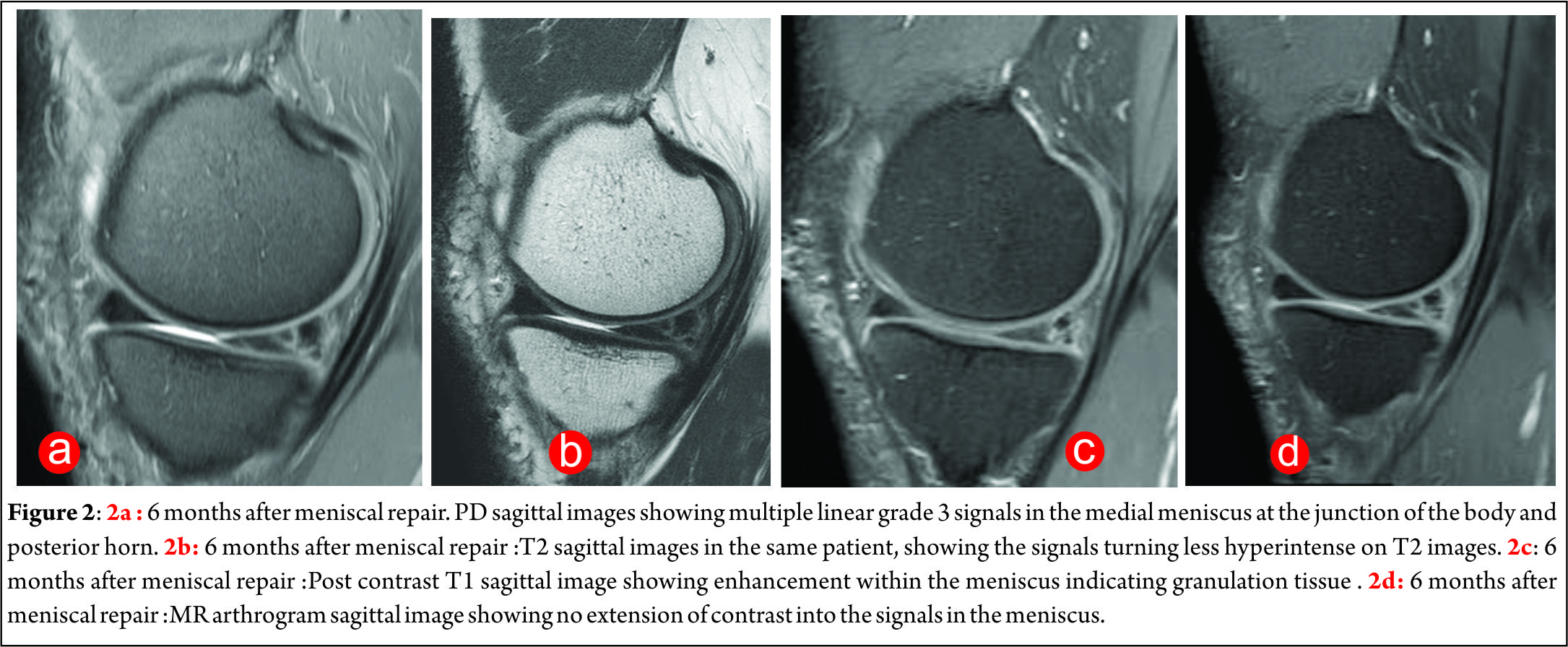
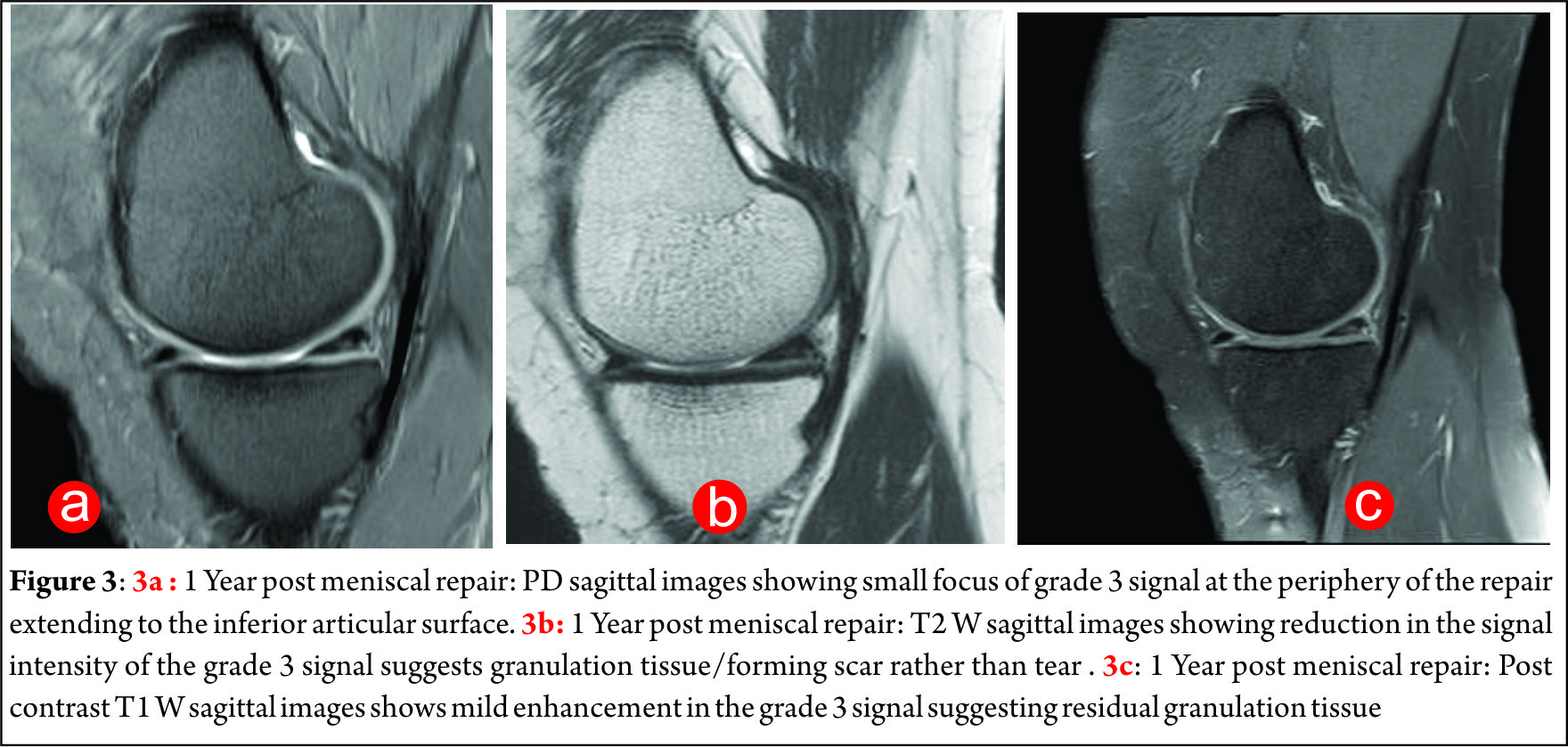
As opposed to in a virgin meniscus, mere presence of a grade 3 signal is not enough to make the diagnosis of a tear. The initial fibrovascular granulation tissue and later mature fibrocartilagenous scar produces increased signal intensity [grade 3] on the intermediate weighted sequences in a healing/healed meniscus [12]. This can cause fallacious interpretation of non- healing of the repair [7, 11, 13, 14] [Fig 1A]. Long segment tears and bucket-handle tears especially may have increased rates of grade 3 signal. This is because of the long injury length, which could induce more fibrocartilaginous scars and result in more grade 3 signals during the healing procedure [15]. Also the repairs with FasT-Fix showed more grade 3 signals than the other 2 repair patterns on the PD images. This is because FasT-Fix is non- absorbable and thus induces more reaction [15]. The signal intensity does reduce over time as the meniscus undergoes healing and may in fact disappear altogether [7]. Thus, diagnosis of meniscal tear by using the usual criterion of linear increased signal intensity extending to the surface on conventional short echo time MR images may lead to a false-positive diagnosis in patients after meniscal repair. Use of the stricter criterion of fluid signal intensity within a linear defect in the meniscus on T2-weighted images has been shown to provide high specificity (88%–92%) but low sensitivity (41%–69%) for tears [13, 16, 17]. The use of this stricter criterion with conventional MR imaging will result in fewer false-positive diagnoses, however, many tears will be missed. Identification of displaced meniscal fragments allows detection of tears with high confidence; however, displaced fragments are only seen in the minority of tears. Further addition of intra-articular contrast increases the sensitivity and specificity of diagnosis of tear[4, 11, 13, 16, 18, 19]. Extension of intra-articular contrast into the grade 3 signal indicates presence of a tear. The various imaging modalities that can be used for evaluation of a post-repair meniscus are as follows:
Conventional MRI
3T [high field strength magnet] and a dedicated knee coil are preferred for imaging as they provide high spatial resolution of the images obtained. The routinely performed conventional MRI sequences are PD [proton density, intermediate] sagittal and coronal, T2 sagittal, PD and T2 axial, T1 sagittal and 3D VISTA. The 3D VISTA sequences are then reformatted into the axial plane to delineate the morphology in the long axis of the meniscus. Presence of mildly hyperintense linear grade 3 signals on PD images is normal for many years after surgery Fig 1A. It represents initial fibrovascular granulation tissue and later fibrocartilagenous mature scarring. This turns less hyperintense on T2 [Fig 1B]. On intravenous administration of contrast, there is enhancement of granulation tissue, which reduces in intensity and extent over the next 12-18 months. [Fig 1C, 2A, 2B, 2C, 3A, 3B, 3C]. MR arthrography has some advantages over conventional MRI. Distension of the joint makes it more likely for the contrast to enter into the tear and delineate it. Lower viscosity of gadolinium compared to synovial fluid makes it more likely to extend into the tear. T1 W images which are used in MR arthrography have a higher signal to noise ratio and this improves spatial resolution [3].

Direct MR arthrography
After the conventional MRI sequences are obtained, contrast [50 cc of gadolinium diluted 1:250 to 1:100] is injected into the knee joint under fluoroscopic guidance and multiplanar T1 W images are obtained thereafter [4]. Intra-articular contrast insinuates into a tear and delineates it on the post contrast T1 W images. This helps to differentiate a tear from a grade 3 signal which is merely a scar tissue.
Indirect MR arthrography
The process of healing of the meniscus can be non- invasively assessed by indirect MRA. [7, 20]. After the conventional MRI sequences are obtained, gadolinium contrast [0.1 mmoles/kg] is injected intravenously and the joint is exercised for 20-25 minutes. After this, T1 W images are obtained in multiple planes [4, 7]. The advantage of this procedure is that it is non –invasive and can be performed by a technician or nursing staff . Also patient compliance is better than for direct arthrography [11]. According to some studies there is no significant difference in diagnostic accuracy between direct and indirect MR arthrography. Indirect MR arthrography is a less-invasive procedure. The presence of a physician and fluoroscopic guidance is not required, making it probably a better imaging approach than direct MR arthrogram [4, 11]. Hantes et al observed that the signal to noise ratio [SNR] of the repaired tear reduces significantly and approximately 50% from 3 to 6 months, and from 6 to 12 months postoperatively, as demonstrated with indirect MR arthrography [7]. However, in comparison to normal meniscus, the SNR of a tear remains 5.5 times higher 12 months postoperatively. In contrast, the reduction of SNR of the repaired tear at conventional MRI was not significant even from 3 to 12 months [7].
Normal findings in a post-repair meniscus on MRI /MRA:
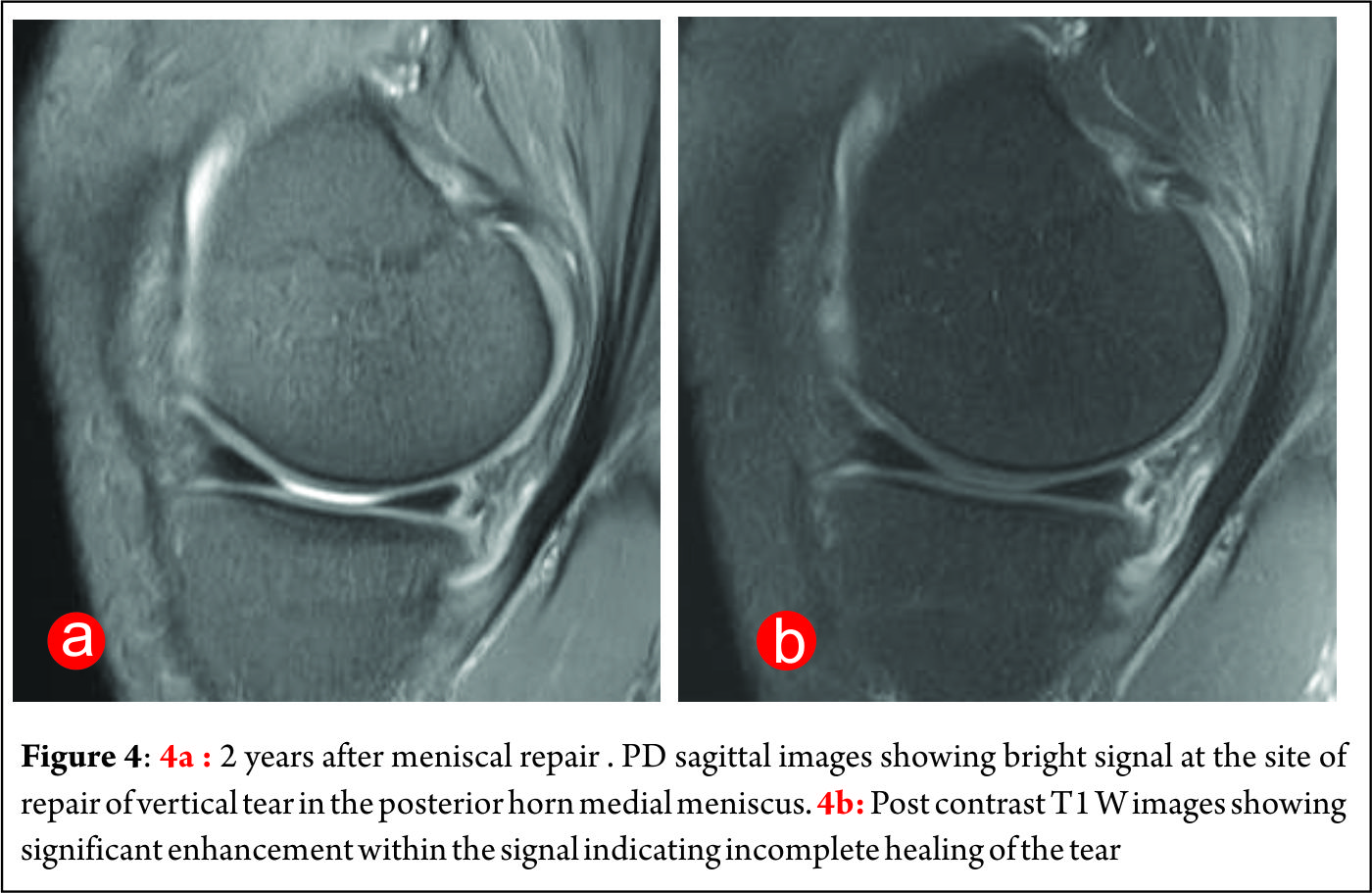
It is important to know what the normal findings seen on an MRI of a post operative /repaired meniscus are, so as not to misinterpret these findings as abnormal or pathological. Grade 3 signals are noted on the intermediate [PD/T1W] sequences extending to the articular surfaces. These may persist for many years after surgery and are attributed to fibrovascular granulation tissue in the initial post operative period and fibrocartilagenous tissue in the later post operative period. [4, 13, 16, 21-24]. These signals reduce in intensity over time. [20, 25]. There is some degree of shrinkage /reduction in the width of the meniscus after meniscal repair. This is different in different segments of the meniscus. Some degree of enhancement is seen within the repair on the immediate post contrast images [for almost 12-18 months post operatively due to the presence of granulation tissue]. The intensity of enhancement reduces over the next 12-18 months. [Fig 2A, 2B, 2C, 3A, 3B, 3C]. There will however not be any extension of contrast into the signal on the MR arthrogram images [7, 8]. Persistence of enhancement in a meniscus 18 months post operatively suggests non-healing of the repair[Fig 4A, 4B] Occasionally a degenerative signal may be seen in a post operative meniscus many years after surgery due to the onset of degenerative changes [26].
Criteria to suggest recurrent/residual tear on MRI /MRA
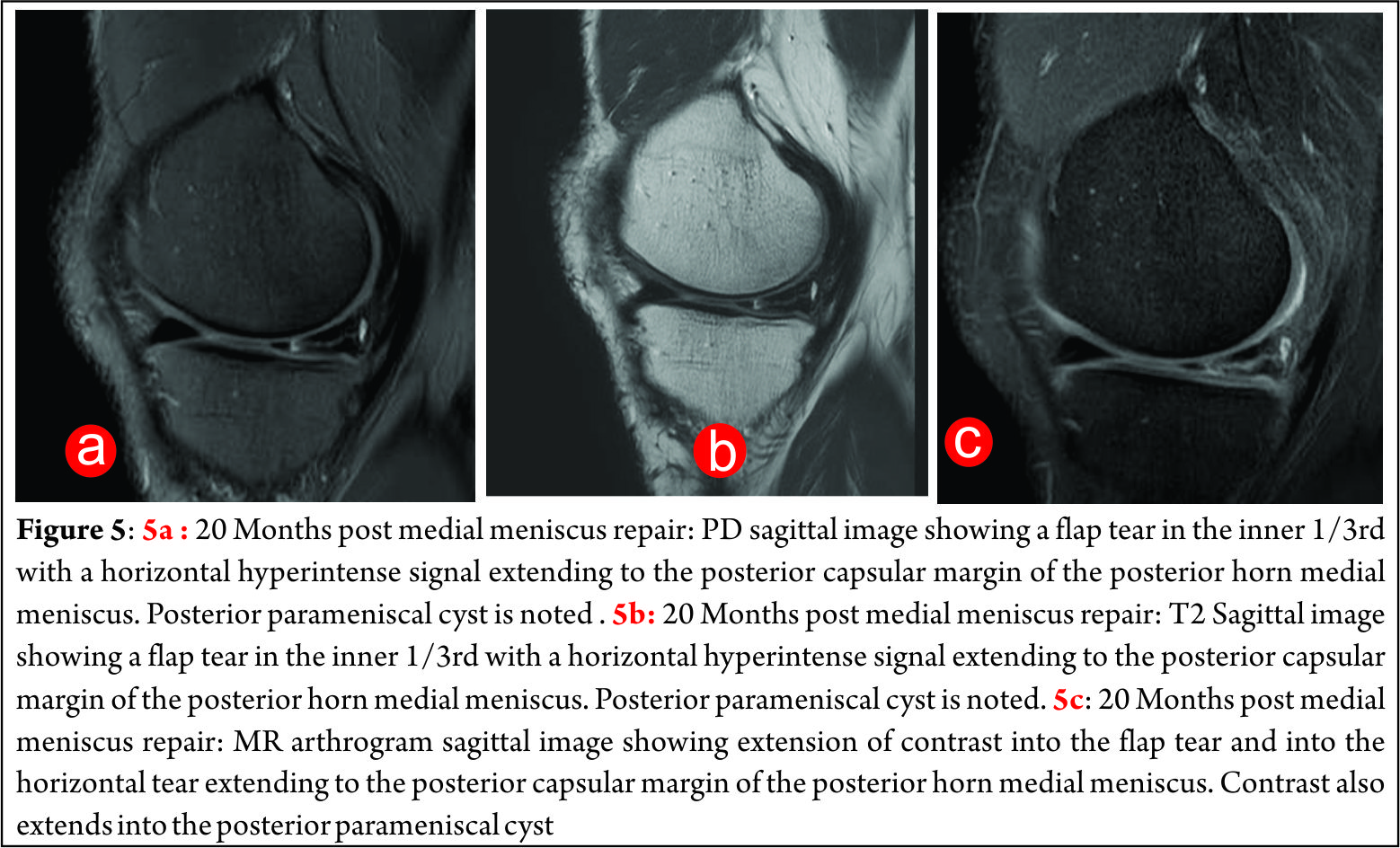
Bright signal seen within the meniscus on the T2 W images is more specific for a recurrent /persistent tear, especially 12 months post operative [3, 13, 16, 17]. After the administration of intra-articular contrast [either directly into the joint or indirectly by the intravenous route, extension of contrast into the signal abnormality on the MR arthrogram adds to the sensitivity and specificity of the diagnosis [Fig 5A, 5B, 5C]. Sometimes displaced meniscal fragment may be identified which is then a definite sign of a retear [16, 27, 28]. The presence of a parameniscal or intrameniscal cyst suggests the presence of a residual /recurrent tear. Presence of abnormal signal intensity at a site distant from the site of original repair indicates the presence of a fresh tear [3]. The healing process can also be classified according to Henning’s criteria, depending on healing in the thickness of the meniscus. A meniscus is considered healed if it heals over the full thickness of the tear, incompletely healing if it was healed over at least 50 % of the thickness of the tear and a failure was defined as healing less than 50 % of the thickness at any point along the length of the tear [29].
NOTE:
Assessment of a post operative meniscus [especially a post-repair meniscus] on MRI is difficult. Comparison with previous MRI studies is essential to know the exact location, extent and morphology of the prior year for interpretation of the signals seen on the post-operative study [11]. Even with addition of intra-articular contrast, the contrast may not enter the tear if the mouth/opening of the tear is very narrow. This will cause a false negative diagnosis.
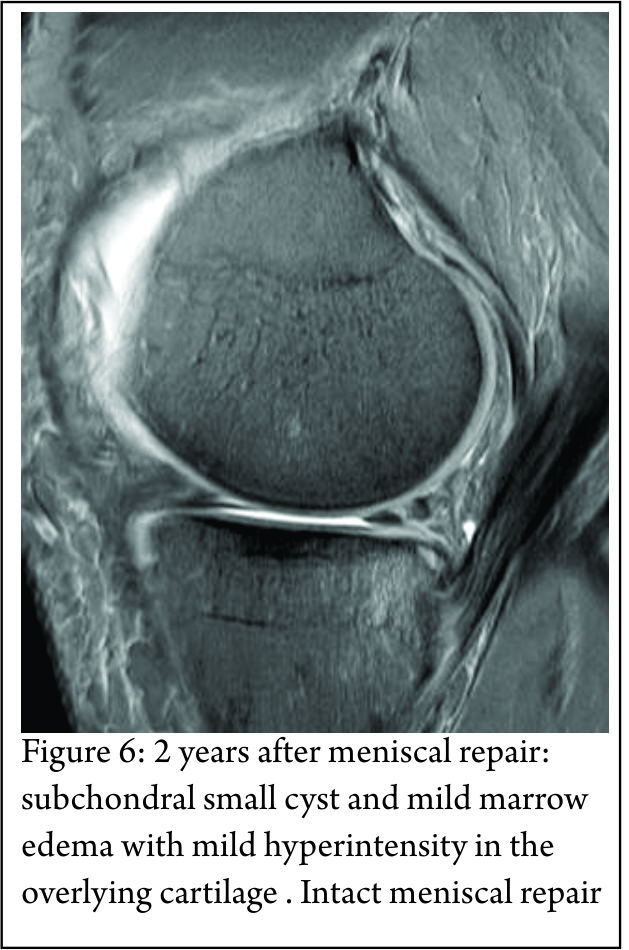
It is also important to remember that not all recurrent pain after meniscal repair surgery is related to the meniscus. Chondral/osseous abnormalities and pes anserine inflammation can also occur and be the cause of pain [4]. [Fig 6]
CT Arthrography
CT arthrography is another modality which may sometimes be used especially when there is non- availability of MRI or in patients in whom MRI is contraindicated. A volume of 10 cc iodinated contrast mixed with1 cc of 0.1%solution of epinephrine is injected under fluoroscopic guidance into the joint space. The patient is then asked to exercise the knee for 20-25 minutes. Thereafter a spiral CT scan is performed and the images acquired are reconstructed in the sagittal and coronal planes [5, 30]. Henning’s criteria for healing on arthro-CT correspond to “thickness” healing criteria. [31]. A meniscus was considered healed if it was healed over the full thickness of the tear. A tear was classified as incomplete healing if healed over at least 50% of the thickness of the tear. A failure was defined as healing<50% of the thickness at any point over the length of the tear.
There are some limitations to the use of CT arthrography. It cannot concomitantly evaluate ACL grafts and osseous abnormalities are not well assessed. The hazard of ionizing radiation and the possibility of complications ensuing from intraarticular injection of iodinated contrast material are also major disadvantages.
Second look arthroscopy
Second look arthroscopy remains the gold standard for assessment of meniscal healing. The disadvantage of this is that it is an invasive procedure and hence patient compliance is less. [23, 32-34].
Conclusions
Meniscal repair is increasingly replacing menisectomy as the treatment of choice especially in young patients in order to avoid early onset of osteoarthrosis. Imaging options such as MRI, MR arthrography and CT arthrography are being used as alternatives to clinical assessment and second look arthroscopy for the evaluation of meniscal repair healing. Conventional MRI has the disadvantage of grade 3 signals persisting for years after surgery even in a healed meniscus. The additional of a T2 W sequence on conventional MR imaging and usage of intra-articular contrast [MR arthrograms, direct and indirect] have increased the specificity, sensitivity and accuracy of diagnosis of unhealed menisci and retears. Second look arthroscopy does however remain the gold standard for the diagnosis of retears, as of date.
References
1. Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011 Oct; 32 (30):7411-7431.
2. McCauley TR. MR Imaging Evaluation of the Postoperative Knee. Radiology 2005; 234:53–61.
3. Recht MP, Kramer J. MR Imaging of the Postoperative Knee: A Pictorial Essay. RadioGraphics 2002; 22:765–774.
4. White LM, Schweitzer ME, Weishaupt D, Kramer J, Davis A, Marks PH. Diagnosis of Recurrent Meniscal Tears: Prospective Evaluation of Conventional MR Imaging, Indirect MR Arthrography, and Direct MR Arthrography. Radiology 2002; 222:421–429.
5. Vande Berg BC, Lecouve FE, Poilvache P, Dubuc JE, Bedat B, Maldague B, et al. Dual-Detector Spiral CT Arthrography of the Knee: Accuracy for Detection of Meniscal Abnormalities and Unstable Meniscal Tears.Radiology 2000; 216:851–857.
6. Pujol N, Panarella L, Tarik Ait Si Selmi, Neyret P, Fithian D, Beaufils P. Meniscal Healing After Meniscal Repair :A CT Arthrography Assessment. The American Journal of Sports Medicine 2008; Vol.36, No.8 :1489-1495.
7. Hantes ME, Zachosa VC, Zibisa AH, Papanagiotoub P, Karahaliosa T, Malizosa KN, Karantanasb AH. Evaluation of meniscal repair with serial magnetic resonance imaging: a comparative study between conventional MRI and indirect MR arthrography. European Journal of Radiology 50 (2004) 231–237.
8. Vance K, Meredick R , Schweitzer ME, Lubowitz JH. Magnetic Resonance Imaging of the Postoperative Meniscus. Arthroscopy 2009; 25, (5): 455-570.
9. Jones HP, Lemos MJ, Wilk RM, Smiley PM, Gutierrez R, Schepsis AA. Two-year follow-up of meniscal repair using a bioabsorbable arrow. Arthroscopy 2002; 18(1):64-69.
10. Lim PS, Schweitzer ME, Bhatia M, et al. Repeat tear of postoperative meniscus: potential MR imaging signs. Radiology 1999; 210:183–8.
11. Vives MJ, Homesley D, Ciccotti MG, Schweitzer ME. Evaluation of recurring meniscal tears with gadolinium-enhanced magnetic resonance imaging. Am J Sports Med 2003;31:868–73.
12. Arnoczky SP, Cooper TG, Stadelmaier DM, Hannafin JA. Magnetic resonance signals in healing menisci: an experimental study in dogs. Arthroscopy 1994; 10:552–7.
13. Farley TE, Howell SM, Love KF, Wolfe RD, Neumann CH. Meniscal tears: MR and arthrographic findings after arthroscopic repair. Radiology 1991; 180:517–522.
14. Bronstein R, Kirk P, Hurley J. The usefulness of MRI in evaluating menisci after meniscus repair. Orthopedics.1992 Feb;15(2):149-52.
15. Miao Y, Yu JK, Ao YF, Zheng ZZ, Gong X, Leung KK. Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med. 2011 ;39(4):735-42.
16. Applegate GR, Flannigan BD, Tolin BS, Fox JM and Pizzo WD. MR diagnosis of recurrent tears in the knee: value of intraarticular contrast material. American Journal of Roentgenology. 1993;161: 821-825.
17. Lim PS, Schweitzer ME, Bhatia M, Giuliano V, Kaneriya PP, Senyk RM, et al. Repeat Tear of Postoperative Meniscus: Potential MR Imaging Signs. Radiology 1999; 210:183–188
18. Vahlensieck M, Peterfy CG, Wischer T, et al. Indirect MR arthrography: optimization and clinical applications. Radiology 1996; 200:249– 54.
19. Drape JL, Thelen P, Gay-Depassier P, Silbermann O, Benacerraf R. Intraarticular diffusion of Gd-DOTA after intravenous injection in the knee: MR imaging evaluation. Radiology 1993; 188:227–34.
20. Toms AP, White LM, Marshall TJ, Donnell ST.Imaging the post-operative meniscus. Eur J Radiol.2005 May ; 54 (2) : 189-98.
21. Pujol N, Nicolas T, Boisrenoult P, Beaufils P. Magnetic Resonance Imaging is not suitable for interpretation of meniscal status ten years after arthroscopic repair. Int Orthop. 2013 Dec; 37(12): 2371–2376.
22. Arnoczky SP, Cooper TG, Stadelmaier DM, Hannafin JA. Magnetic resonance signals in healing menisci: an experimental study in dogs. Arthroscopy 1994;10:552–7.
23. Eggli S, Wegmüller H, Kosina J, Huckell C, Jakob RP. Long term results of arthroscopic meniscal repair. Am J Sports Med 1995; 23:715– 20.
24. Muellner T, Egkher A, Nikolic A, Funovics M, Metz V. Open meniscal repair: clinical and magnetic resonance imaging findings after 12 years. Am J Sports Med 1999; 27:16–20.
25. Mustonen AO, Tielinen L, Lindahl J, Hirvensalo E, Kiuru M, Koskinen SK. MRI of menisci repaired with bioabsorbable arrows. Skeletal Radiol. 2006; 35(7):515-521.
26. Steenbrugge F, Verstraete K , Verdonk R.Magnetic reasonance imaging of the surgically repaired meniscus A 13-year follow-up study of 13 knees. Acta Orthop Scand 2004; 75 (3): 323–327 .
27. Sciulli RL, Boutin RD, Brown RR, Nguyen KD, Muhle C, Lektrakul N , Resnick D et al .Evaluation of the postoperative meniscus of the knee: a study comparing conventional arthrography, conventional MR imaging, MR arthrography with iodinated contrast material, and MR arthrography with gadolinium-based contrast material. . Skeletal Radiol. 1999; 28(9):508-514.
28. Magee T, Shapiro M, Rodriguez J, Williams D. MR Arthrography of Postoperative Knee: For Which Patients Is It Useful? Radiology. 2003 Oct; 229(1):159-63.
29. Popescu D, Sastre S, Garcia AI, Tomas X, Reategui D, Caballero M. MR arthrography assessment after repair of chronic meniscal tears. Knee Surg Sports Traumatol Arthrosc. 2015 Jan;23(1):171-7
30. Mutschler C, Vande Berg BC, Lecouvet FE, Poilvache P, Dubuc JE, Maldague B, Malghem J. Postoperative Meniscus: Assessment at Dual–Detector Row Spiral CT Arthrography of the Knee. Radiology 2003; 228:635–641.
31. Pujol N , Panarella L, Selmi TA, Neyret P, Fithian D, Beaufils P. Meniscal healing after meniscal repair: a CT arthrography assessment. Am J Sports Med. 2008 ; 36(8):1489-95.
32. Henning CE. Arthroscopic repair of meniscus tears. Orthopedics 1983:6:1130-1132.
33. Henning CE, Lynch MA, Clark JR. Vascularity for healing of meniscus repairs. Arthroscopy 1987; 3 (1): 13-8.
34. Buseck MS, Noyes FR: Arthroscopic evaluation of meniscal repairs after anterior cruciate ligament reconstruction and immediate motion. Am Sports Med 1991;19: 489–494.
| How to Cite this article:. Patil AS, Chandorkar AH. Imaging of Meniscus Repair and Healing : A Review of Current Trends/ Literature. Asian Journal of Arthroscopy Aug – Nov 2016;1(2):23-27. |