Sundararajan S R, Jain Sachin Ramesh, S Rajasekaran
Volume 1 | Issue 1 | April – Jun 2016 | Page 38-42
Author: Sundararajan S R [1], Jain Sachin Ramesh [1], S Rajasekaran [1]
[1] Ganga Hospital, 313, MTP road, Coimbatore , Tamilnadu, India Pin code – 641043
Address of Correspondence
Dr Sundararajan S R
Ganga hospital, 313, MTP road, Coimbatore , Tamilnadu, India,
Pin code – 641043
Email id – sundarbone70@hotmail.com
Abstract
Purpose: The main purpose of the study was to evaluate arthroscopic biopsy results and MRI findings in monoarticular joint synovitis with emphasis on differentiation between tuberculosis and rheumatoid cases using MRI features by Choi et al.
Materials and methods: Between 2010 and 2014, 34 patients were retrospectively analyzed from our database. Clinical history, MRI findings, arthroscopy findings & biopsy reports were evaluated. Findings of Choi et al was used to correlate MRI and biopsy results between rheumatoid and tuberculosis cases. Ability of MRI in diagnosing other cases like PVNS, hemangioma was also evaluated. Samples obtained from biopsy were sent to two laboratories in 23 of our cases where MRI was suggestive of infective or inflammatory etiology.
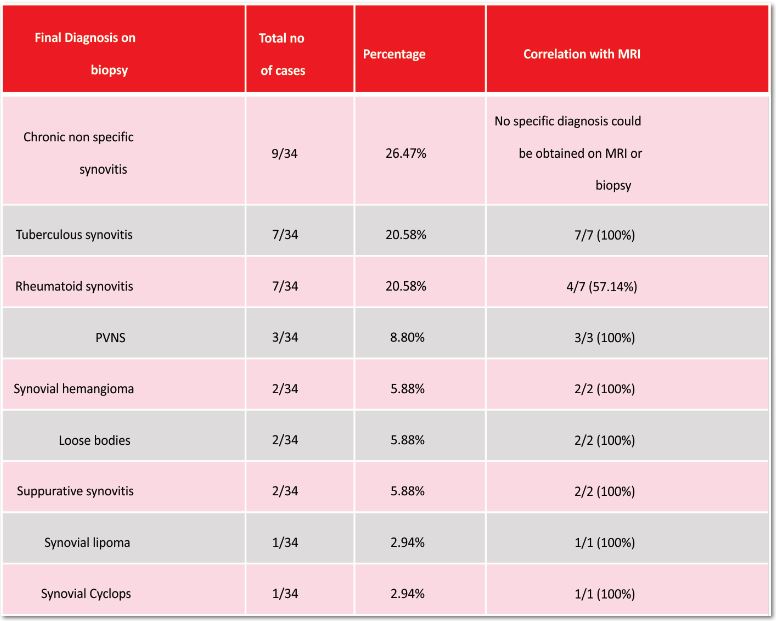
Results: Out of 34, 9(26.47%) cases were of chronic nonspecific synovitis, 7(20.58%) cases of tuberculous synovitis, 7(20.58%) cases of rheumatoid synovitis, 3(8.8%) cases of PVNS, 2(5.88%) cases of Synovial hemangioma, and 6 others. Out of 34, tissue biopsy diagnosis was made in 25(73.53%) and MRI diagnosis was obtained in 22/34 (65%) of our patients. Using features described by Choi et al, 100% of tuberculosis cases and 57.14% of rheumatoid cases were diagnosed on MRI. A mismatch of 4/23(17.4%) was found between the reports from two recognized labs.
Conclusions: Arthroscopic biopsy and MRI are reliable techniques, with better success rate in the diagnosis of monoarticular synovitis of unknown etiology. Choi et al’s MRI recommendations are reliable in differentiating between infective or inflammatory etiology.
Keywords: Synovitis, Monoarticular, Undifferentiated, arthroscopic biospy
Introduction
Monoarticular joint synovitis of undifferentiated etiology (1), presents with complaints of pain and swelling which is not responding to anti-inflammatory treatment. Diagnosis and approach to treatment in such cases is very important for satisfactory clinical results. Arthroscopy is the preferred mode for biopsy (2-7) and provides macroscopic evaluation(3,8,9) of the monoarticular joint disease. Early diagnosis of tubercular synovitis is important to prevent joint damage(7) within few days to weeks. Similarly, inflammatory synovitis like rheumatoid synovitis also carries a prognostic significance if diagnosed early and treated(8).
Plain radiograph in early synovial disease usually remains normal for at least 6 to 12 months after symptom onset(10). MRI is a highly sensitive tool to evaluate early undifferentiated synovitis and guide the management plan(11,12). It gives the extent of synovial hypertrophy(12) with sites of increased activity with gadolinium enhancement for directing biopsy(12,13). MRI features described by Choi et al(14), where they considered synovial thickening, bone erosions, rim enhancement at bone erosions, soft tissue edema and extraarticular cystic masses for differentiating tubercular and rheumatoid synovitis.
Our hypothesis is that MRI can diagnose the specific etiology, especially the tubercular and rheumatoid synovitis, in monoarticular joint synovitis of undifferentiated origin using the MRI features described by Choi et al (14).
Methods
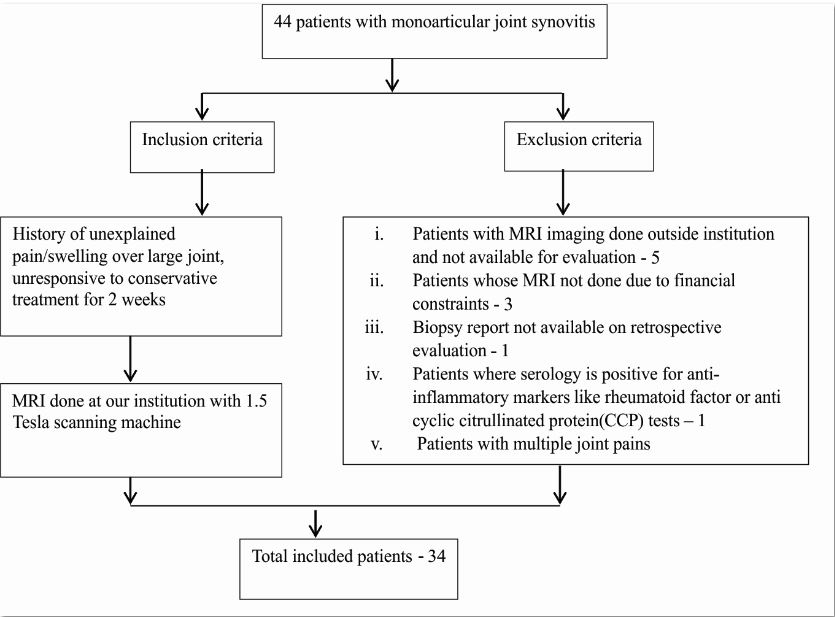
The study was approved by ethics committee of our institution. Between 2010 and 2014, 34 patients were retrospectively analyzed from our database using the inclusion and exclusion criteria (Flowchart 1). Clinical history, MRI findings, arthroscopy findings and biopsy reports were evaluated. Blood investigation like Rheumatoid factor, anti cyclic citrullinated protein (CCP) was used to diagnose inflammatory arthritis like rheumatoid and those cases were excluded from our study. If a patient presenting to our center for the first time without any waiting period then our policy is to give 2 weeks of anti-inflammatory medications and if symptoms don’t subside than we go ahead with other investigation of MRI, blood tests and immediate arthroscopic biopsy depending on MRI reports. If patient has already has waited for more than 2 weeks then we directly investigate with MRI, blood tests and go ahead with arthroscopic treatment.
Out of 34 joints, 26 knees, 5 ankles, 2 hips and 1 shoulder joint were included. Out of 34 patients 22 were males and 12 females between ages 9 years and 70 years. According to Choi et al(14) as described in table 1, if uniform synovial thickening, large size of bone erosion, and extra articular cystic masses more frequent and more numerous, then tubercular synovitis(14) and if more the degree of synovial hypertrophy without associated findings were present then diagnosis of rheumatoid synovitis(14) was considered. We used these findings to correlate MRI and biopsy results retrospectively between rheumatoid and tuberculosis cases.
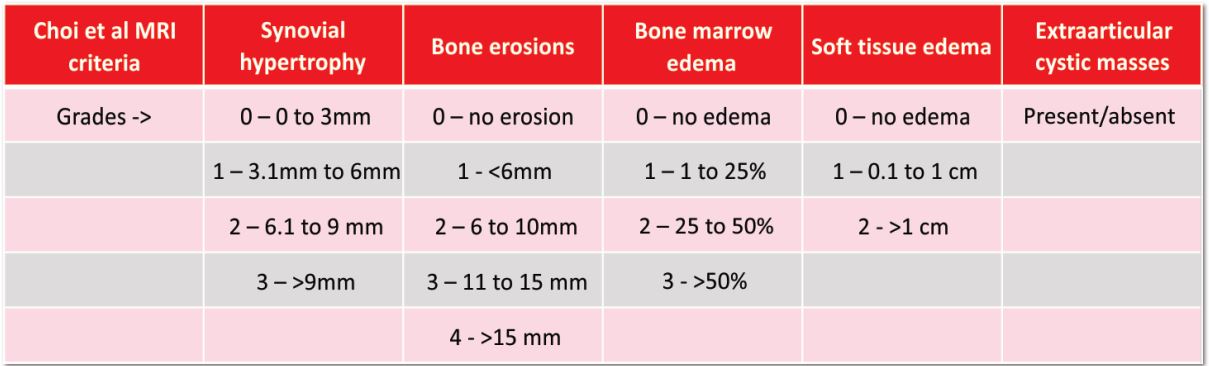
Table 1: Criteria and grading on MRI based on Choi et al (14) to differentiate between rheumatoid and tubercular synovitis
Arthroscopic evaluation was performed by a single senior arthroscopy consultant of our institution. On arthroscopic evaluation, joint was thoroughly inspected through standard portals. Macroscopic evaluation of the joint done and the suspected area of increased activity were chosen for biopsy. At least 6 different sites in the joint was considered for biopsy, material was packed in formalin filled glass bottle and sent for histopathological examination. Arthroscopic partial or subtotal synovectomy was done if needed. Biopsy samples were sent to two different laboratories only when MRI diagnosis showed chronic synovitis of infective or inflammatory etiology, where the cause was doubtful. To be sure of the diagnosis, biopsy material was sent in these patients by two experienced senior pathologist. . Depending upon the biopsy results further treatment was initiated. No prophylactic anti-tubercular treatment was started as biopsy results usually arrived in a week for definitive treatment. Arthroscopic biopsy samples were sent to two labs for evaluation only where diagnosis of inflammatory or infective origin was doubtful on MRI in 23 out of 34 cases
Results
In our case series, Out of 34, 9(26.47%) cases were of chronic nonspecific synovitis, 7(20.58%) cases of tuberculous synovitis, 7(20.58%) cases of rheumatoid synovitis, 3(8.8%) cases of PVNS, 2(5.88%) cases of Synovial hemangioma, and 6 others. Out of 34, tissue biopsy diagnosis was made in 25(73.53%) and MRI diagnosis was obtained in 22/34 (65%) of our patients. Using features described by Choi et al, 100% of tuberculosis cases and 57.14% of rheumatoid cases were diagnosed on MRI (Table 1). There was a mismatch in biopsy results among 4 (17.4%) out of the 23 cases that were sent to two recognized laboratories simultaneously.
Discussion
Monoarticular synovitis of unexplained origin (5) needs a series of tests like blood investigation, MRI and biopsy to find out the causal factor. Effectiveness of arthroscopic biopsy in the diagnosis of monoarticular synovitis was discussed (4,6,17) earlier. We attempted to determine the same in this series along with effectiveness of MRI diagnosis. Conditions like synovial hemangioma and PVNS is done quite accurately (19,20,21) using MRI, but there is difficulty in diagnosing or differentiating infective versus inflammatory etiology. Choi et al(14) was the first to evaluate and differentiate these two conditions using MRI. We evaluated the suggested guidelines in this study.
Arthroscopy plays an important role in diagnosis(2,4,15). Major use is in the patients presenting with unexplained knee pain whose symptoms are disproportionate to the radiologic features or refractory to standard course of medical treatment(2). Arthroscopic synovial biopsy is considered as the ‘gold standard'(16) for biopsy in monoarticular joint synovitis. Arthroscopy is an excellent tool to visualize the synovium macroscopically(3,8,9), evaluate the villi precisely and obtain biopsy from site correlating with clinical findings for microscopic evaluation3,6,8. Macroscopic evaluation of normal synovium looks bland and devoid of villi, granularity or increased vascularity(8).
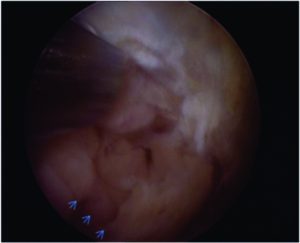
Figure 1a: Arthroscopic view of knee joint through anterolateral portal showing synovial hypertrophy (small arrows) in the suprapatellar fossa with 30 degree lens and camera facing 4 ‘o clock position.

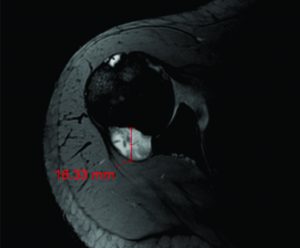
Figure 1b: MRI showing extensive bony edema(26.90mm), synovial hypertrophy(11.78mm), multiple bony erosions(14.44mm), and extra articular cystic masses(*) favoring diagnosis of tuberculous synovitis.
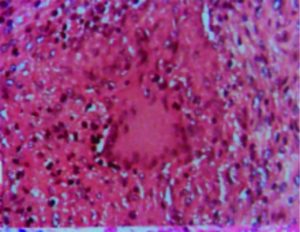
Figure 1c: Histopathology findings showing epitheloid cells and granulomatous inflammation (arrow) suggestive of tuberculosis.
Arthroscopic findings can alter or add to the treatment plan which includes surgical tissue resection or medical treatment like Disease Modifying Anti-rheumatic Drugs (DMRD’s) to the current treatment(2). Goeb et al(22) suggested that early diagnosis and early treatment initiation in patients with inflammatory arthritis can be possible by precise arthroscopic biopsy sample from the most representative pathological areas. Chen et al(14) evaluated the role of arthroscopy in unilateral knee arthritis where they accurately diagnosed 71 cases and 3 cases were undiagnosable(4). They reported 39/74 (52.9%) cases as rheumatoid arthritis4. In our study, despite thorough arthroscopic and microscopic evaluation, we were not able to accurately diagnose in 26.47% of the patients, which were finally diagnosed as chronic non specific synovitis. Chronic non specific synovitis is also known as monoarthritis of unknown origin (5), 80% of these can go into complete remission over a period of two years(5) with just conservative treatment.
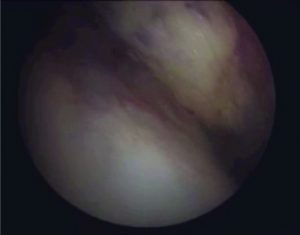
Figure 2a: Arthroscopic view of knee joint through anterolateral portalshowing reddish brown tumor with telangiectatic arterioles suggestive of hemangioma(H) in the lateral aspect of suprapatellar fossa with 30 degree lens and camera facing 12 ‘o clock position.

Figure 2b: Arthroscopic biopsy done through the anterolateral portal from multiple sites with basket punch. Note bleeding from the tumor site (arrow).
As definitive treatment with antitubercular medication is available, diagnosis of early tuberculous synovitis is very essential to prevent cartilage damage. Arthroscopic definitive tissue diagnosis and timely treatment helps in achieving excellent results in 3 – 4 months period (7), with complete symptomatic relief and full joint function restoration(7). Early rheumatoid arthritis carries a prognostic value as disease modifying agents can be introduced, which can reduce the aggressiveness of the disease by inhibiting the progressive structural damage (8). In inflammatory synovitis like early rheumatoid arthritis complete remission or marked improvement is seen in most of the patients(11,15,18).
Out of 34 cases, 23 cases had synovial hypertrophy arthroscopically for which partial or subtotal synovectomy was performed to aid in clinical remission. In case of pigmented villonodular synovitis and synovial hemangioma, MRI guides the diagnosis in all the patients following which arthroscopic extended synovectomy and arthroscopic excision is the preferred treatment(19,20,21) which was performed in our 4 cases.
MRI is a highly sensitive tool for evaluation of patients presenting with undifferentiated synovitis(1). It can detect bony edema, cartilage erosions also when combined with gadolinium enhancement, degree of synovial thickening (pannus) and intraarticular lesions can be picked up (1). In MRI, to differentiate between infective or inflammatory etiology is very difficult. But the extent of synovial hypertrophy, articular cartilage damage and other findings like cartilaginous loose bodies which are not visible on plain radiograph can be detected. Treatment plan can be based upon MRI to guide the site for arthroscopic biopsy, to have a baseline value of synovial hypertrophy if there is recurrence after synovectomy. MRI diagnosis in cases like synovial hemangioma and Pigmented villonodular synovitis (PVNS)(19,20,21) is accurate, as observed in this study too, where extended synovectomy can be planned preoperatively to avoid recurrence. However in a case report by Lee et al (23), where MRI suggested a diagnosis of Pigmented villonodular synovitis due to the hemosiderin deposits and a nodular mass around the knee joint but biopsy revealed it to be tuberculosis. They suggested that the first step in diagnosis of tuberculous knee arthritis is to have high index of suspicion (23). So, even biopsy remains the main means of diagnosis even in such cases.
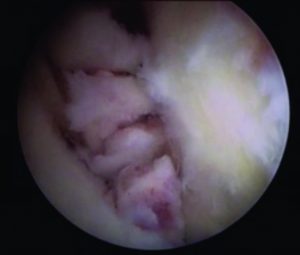
Figure 2c: Piecemeal excision (arrow heads) of the tumor done with arthroscopic scissors through the anterolateral portal with 30 degree lens and camera facing 12′ o clock position.
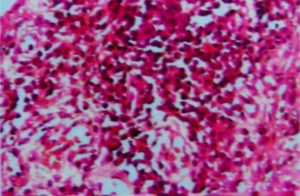
Figure 3b: Histopathology after arthroscopic biopsy of the same shoulder, showing synoviothelial hyperplasia (arrow). Perivascular aggregates of plasma cells with russel bodies (circled) suggestive of rheumatoid synovitis
Overall, MRI agreed with biopsy in 22/34 (65%) of our patients. On using MRI features for finding rheumatoid and tuberculous synovitis, tuberculosis was diagnosed in 7/7(100%) and rheumatoid in 4/7(57.14%) of the cases (Table 2).
Gadolinium enhancement was used in 3 (2 cases were rheumatoid and 1 case was tuberculosis) out of 14 of our patients with tuberculosis and rheumatoid. Enhancement of bone and synovium and also the rim enhancement was similar in both the scenarios. This led us look for other factors in these cases to differentiate between them. Lymph nodes were enlarged in tuberculosis as compared to none in rheumatoid. Also the erosions were multiple and large in tuberculosis as compared to rheumatoid cases. Overall, it was the combination of extensive synovial hypertrophy, multiple large bony erosions, extensive edema, extraarticular mass and enlarged lymph nodes which favored the diagnosis of tuberculosis. Also, synovial hypertrophy with minimal erosion, mild to moderate edema, with no extraarticular masses and no enlarged lymph nodes favored the diagnosis of rheumatoid. Further evaluation for the need of gadolinium contrast agent is needed to assess its real use in differentiating these two conditions.
Arthroscopic biopsy samples were sent to two labs for evaluation in 23 out of 34 cases. Out of which 20 reports matched each other. There was disagreement in 4 out of 23 (17.4%) cases. Out of 4 cases, 3 cases were reported by the lab as chronic non specific synovitis and 1 case of suppurative synovitis which was diagnosed by other lab as 3 cases of rheumatoid and 1 case of tuberculous synovitis, respectively. Implications of correct diagnosis are well known, especially in the case of tuberculosis where there is specific treatment available and complete remission is possible, if it is missed, complete destruction of the joint is inevitable. Therefore it is important to send biopsy samples to at least two laboratories that can increase the probability of correct diagnosis in patients.
Limitation of the study
Several limitations must be taken into consideration in this study. Firstly, the sample size of our study group is small and multiple joints were included, because of the rarity in monoarticular synovitis cases in general, but still it is better than most of the other studies. Secondly, analysis of the MRI was done by single experienced radiologist at our institution. So, effects of interobserver variability could not be assessed in this study. Thirdly, gadolinium enhancement was not performed on every case as we were in initial stages to give enhancement to monoarticular joint synovitis cases before this study was considered, so Choi et al.’s criteria couldn’t be replicated to the exact similarity. Finally, only 23 cases (out of 34) were sent to two laboratories, further reducing the sample size, because of the institute policy to send them to two labs only where diagnosis of inflammatory or infective origin was doubtful on MRI.
Conclusion
Arthroscopic biopsy and MRI both are reliable techniques, with better success rate in the diagnosis of monoarticular synovitis of unknown etiology. Choi et al’s MRI recommendations may aid in differentiating between infective or inflammatory etiology of monoarticular joint synovitis.
References
1. Yasser E, Yasser R. The diagnostic dilemma of undifferentiated inflammatory synovitis of the knee joint/joints: a comprehensive approach. APLAR Journal of Rheumatology 2007 Sep; 10(3):182–189
2. O’Rourke KS, Ike RW. Diagnostic arthroscopy in arthritis patient. Rheum Dis Clin North Am. 1994 May; 20(2):321-42
3. Kurosaka M, Ohno O, Hirohata K. Arthroscopic evaluation of synovitis in the knee joints. Arthroscopy. 1991; 7(2):162-70
4. Chen GQ, Zhang HW, Li ZF,Guo DM, Yu YT. Significance of arthroscopy in the diagnosis of unilateral knee arthritis. Zhonghua Yi Xue Za Zhi. 2010 Jun15; 90(23):1615-7.
5. Scherer T, Kieser C, Gerber H. Assessment and course of 110 patients with monoarthritis. Ther Umsch. 1989 Apr; 46(4):258-64
6. Schulte E, Fisseler-Eckhoff A, Muller KM. Differential diagnosis of synovitis. Correlation of arthroscopic-biopsy to clinical findings. Pathologe. 1994 Feb; 15(1):22-7
7. Cai D, Chen Y, Rong L. Arthroscopy in diagnosis and treatment of tuberculous synovitis. Zhonghua Jie He He Hu Xi Za Zhi. 1998 May; 21(5):276-7
8. Mihir D Wechalekar, Malcolm D Smith. Utility of arthroscopic guided synovial biopsy in understanding synovial tissue pathology in health and disease states. World J orthop 2014 Nov;5(5):566-573
9. Masahiro K, Osamu O, Kazushi H. Arthroscopic evaluation of synovitis in knee joints. Arthroscopy. 1991;7(2):162-170
10. Van der Heijde DM. Plain X-rays in rheumatoid arthritis: overview of scoring methods, their reliability and applicability. Baillieres Clin Rheumatol. 1996 Aug;10(3):435-53
11. M ostergaard, B Ejbjerg, M Stoltenberg et al. Quantitative magnetic resonance imaging as marker of synovial membrane regeneration and recurrence of synovitis after arthroscopic knee joint synovectomy: a one year follow up study. Ann Rheum Dis 2001;60:233-236
12. F.M.McQueen. Magnetic resonance imaging in early inflammatory arthritis: what is its role? Rheumatology 2000;39:700-706
13. Matthew A., Doris E., Mark A. MR imaging of synovial disorders of the knee: An update. Radiologic Clinics Of North America 2007;45:1017-1031
14. Jung-Ah Choi, Sung Hye Koh et al. Rheumatoid arthritis and tuberculous arthritis: Differentiating MRI features. American Journal of Roentgenology 2009 Nov;193(5):1347-1353
15. GAO Jun, GAO Chun-Sheng, GAOYa-zhou et al. Clinical study on arthroscopic examination in diagnosis and treatment of knee synovitis. Journal of clinical and experimental medicine 2013-09
16. Smith MD, Baeten D et al. Standardisation of synovial tissue infilterate analysis: how far we have come? How much further do we need to go? Ann Rheum Dis 2006;65:93-100
17. Onis Singhal, Viplesh kaur et al. Arthroscopic synovial biopsy in definitive diagnosis of joint diseases: An evaluation of efficacy and precision. International Journal of applied and basic medical research, 2012 Jul-Dec;2(2)
18. Ayral X, Bonvarlet JP et al. Arthroscopy-assisted synovectomy in the treatment of chronic synovitis of the knee. Revue du Rhumatisme, 1997,64(4):215-226
19. Rochwerger A, Groulier P et al. Pigmented villonodular synovitis of the knee. Treatment results in 22 cases. Revue de Chirurgie Orthopedique et Reparatrice de L’appareil Moteur, 1998; 84(7):600-606
20. Alessandro De Ponti, Valerio Sansone et al. Result of arthroscopic treatment of Pigmented villonodular synovitis of the knee. Arthroscopy, 2003 Jul-Aug;19(6):602-607
21. Jeung-Tak Suh, Sang-Jin Cheon, Sung-Jong Choi. Arthroscopy, 2003 Sep,19(7):e77-e80
22. Goeb V, Walsh CA, Reece RJ, et al. Potential role of arthroscopy in the management of inflammatory arthritis. Clin Exp Rheumatol, May-June 2012, 30(3) p429-35
23. Lee DH, Lee DK, Lee SH, et al. Tuberculous arthritis of knee joint mimicking pigmented villonodular synovitis. Knee Surg Sports Traumatol Arthrosc, May 2012, 20(5) p937-40
| How to Cite this article:. Sundararajan SR, Jain SR, Rajasekaran S. Arthroscopic Biopsy and MRI Diagnosis in Monoarticular Joint Synovitis of Undifferentiated Origin – A retrospective study in 34 cases . Asian Journal of Arthroscopy Apr- June 2016;1(1):38-42 . |