Sachin Tapasvi, Anshu Shekhar
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 19-22
Author: Sachin Tapasvi[1], Anshu Shekhar[1]
[1] The Orthopaedic Speciality Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004.
Address of Correspondence
Dr Sachin Ramchandra Tapasvi
The Orthopaedic Speciality Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004
Email: stapasvi@gmail.com
Abstract
Meniscus tears are common knee injuries presenting to an arthroscopy surgeon. Repairing the meniscus to salvage knee function and biomechanics is indicated where ever possible, since the problems after meniscectomy are well established now. Inside-out meniscus repair is a very useful technique to repair tears in the posterior and middle third of both menisci. Proper adherence to technique and safety incisions reduce the risks and complications to almost the level of an all-inside meniscus repair. The technique allows precise placement of sutures, causes minimal meniscus tissue trauma, has produced good healing rates, is cost-effective and is basically, an indispensable tool in the armamentarium of any knee surgeon.
Key Words: Meniscus, Meniscus repair, Inside-out, Safety incision, Complications.
Introduction
Meniscus injuries are one of the most common findings in an orthopaedic practice. These injuries lead to a devastating effect on knee dynamics ultimately leading to arthritis. Studies by Fairbanks [1] suggest that the contact stresses after meniscectomy increase considerably leading to symptoms and knee dysfunction. The main function of meniscus, which is to increase surface area for contact of femur over tibia and also to act as a shock absorber for impact activities makes it mandatory to try and save the meniscus whenever possible. Since then the main focus of arthroscopists is to repair and preserve the meniscus. Ikeuchi described the first technique of meniscus repair in Tokyo in 1979 [2]. Over the years, many surgeons have developed techniques for meniscus repairs. The focus of this article is to have an overview of outside-in repair technique for meniscus repair. The outside-in meniscus repair is basically a technique where suture material is passed from outside the knee, retrieved inside the joint and then looped around the tear, again tunneled outside the joint where free ends are tied over the joint capsule. This technique requires the least expensive material and also gives the surgeon modularity to modify the technique to his liking. Many modifications have been done to reduce the cost and simplify the procedure which we will be looking at in details.
Indications
Meniscus repair probability depends on site, size and type of tear. The ideal indication of outside-in meniscus repair is vertical or longitudinal tear in peripheral third of meniscus in a young patient with a stable knee or if the patient is going to have a concomitant ligament reconstruction. For outside-in technique, because we insert a sharp instrument blindly into the joint, the indications are
1: Anterior horn tears
2: Vertical and Longitudinal tears in anterior 2/3rd of meniscus.
* Posterior horn tears may also be tackled by outside-in technique but it has a risk of neuro-vascular injury.
Techniques
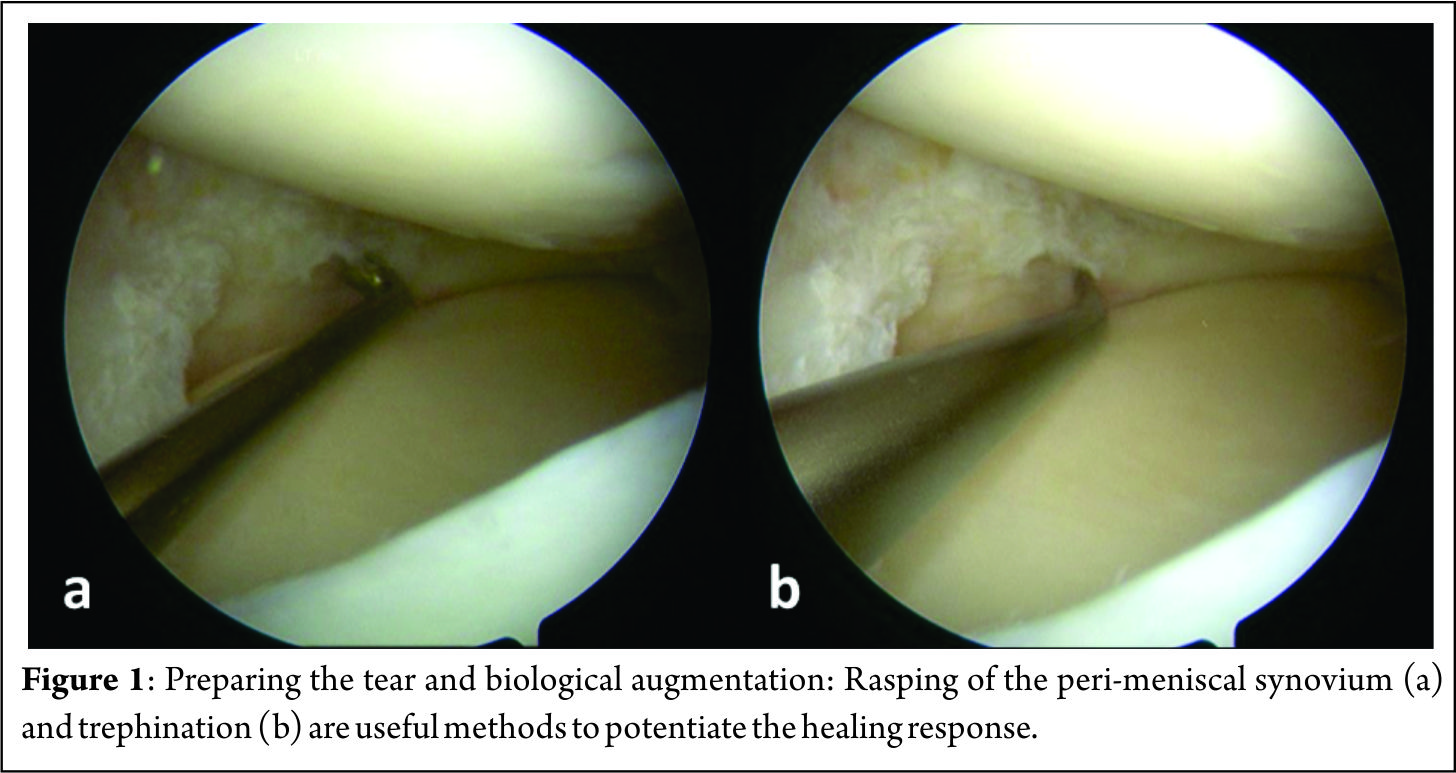
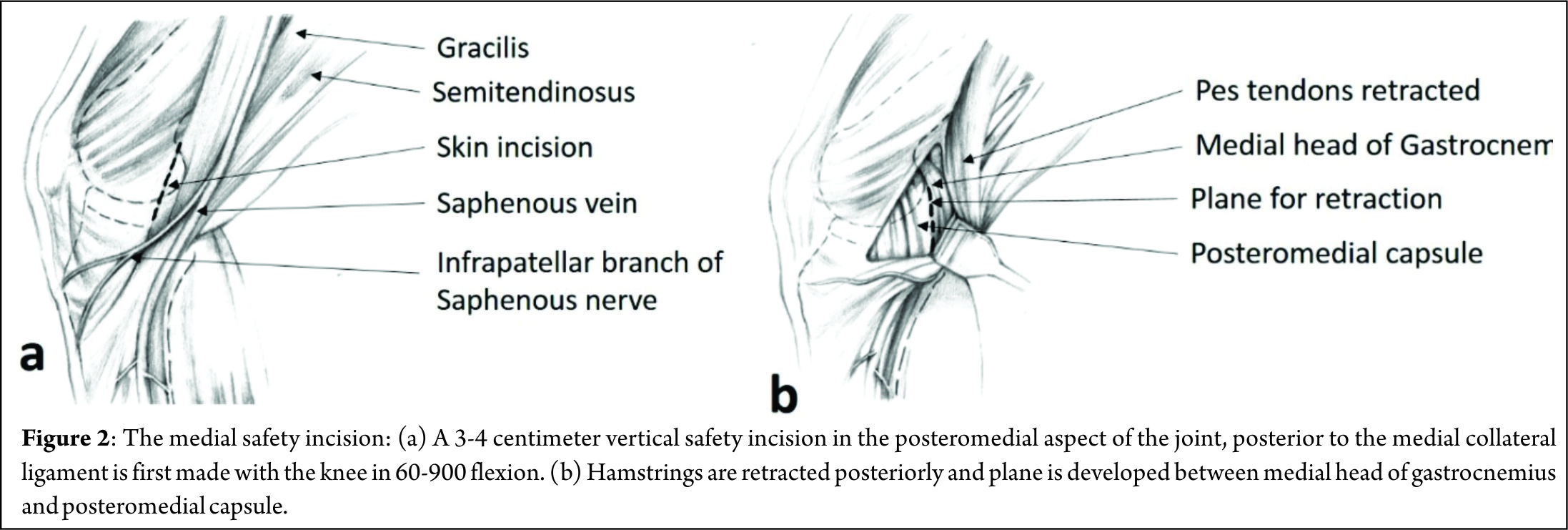
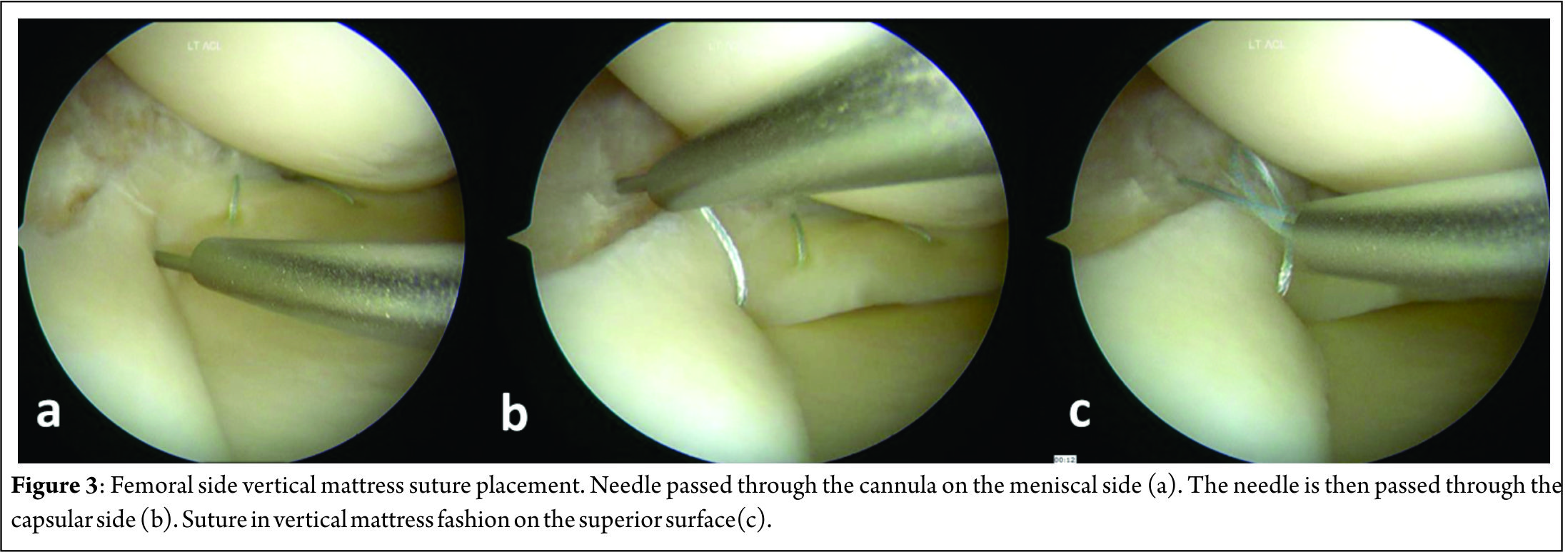
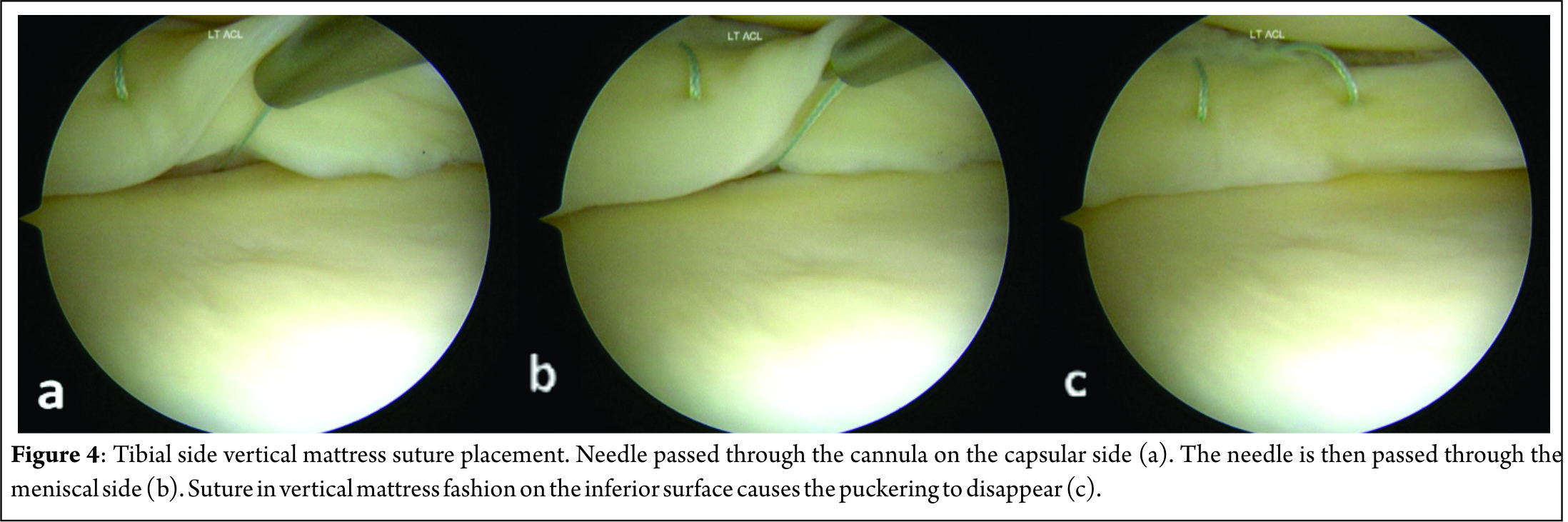
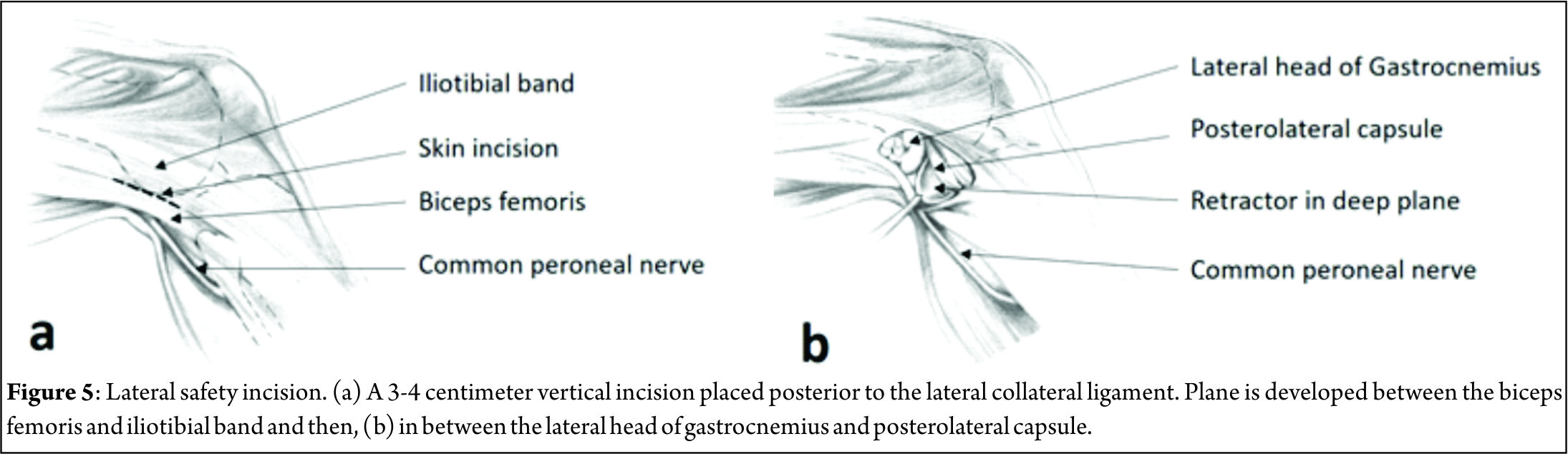
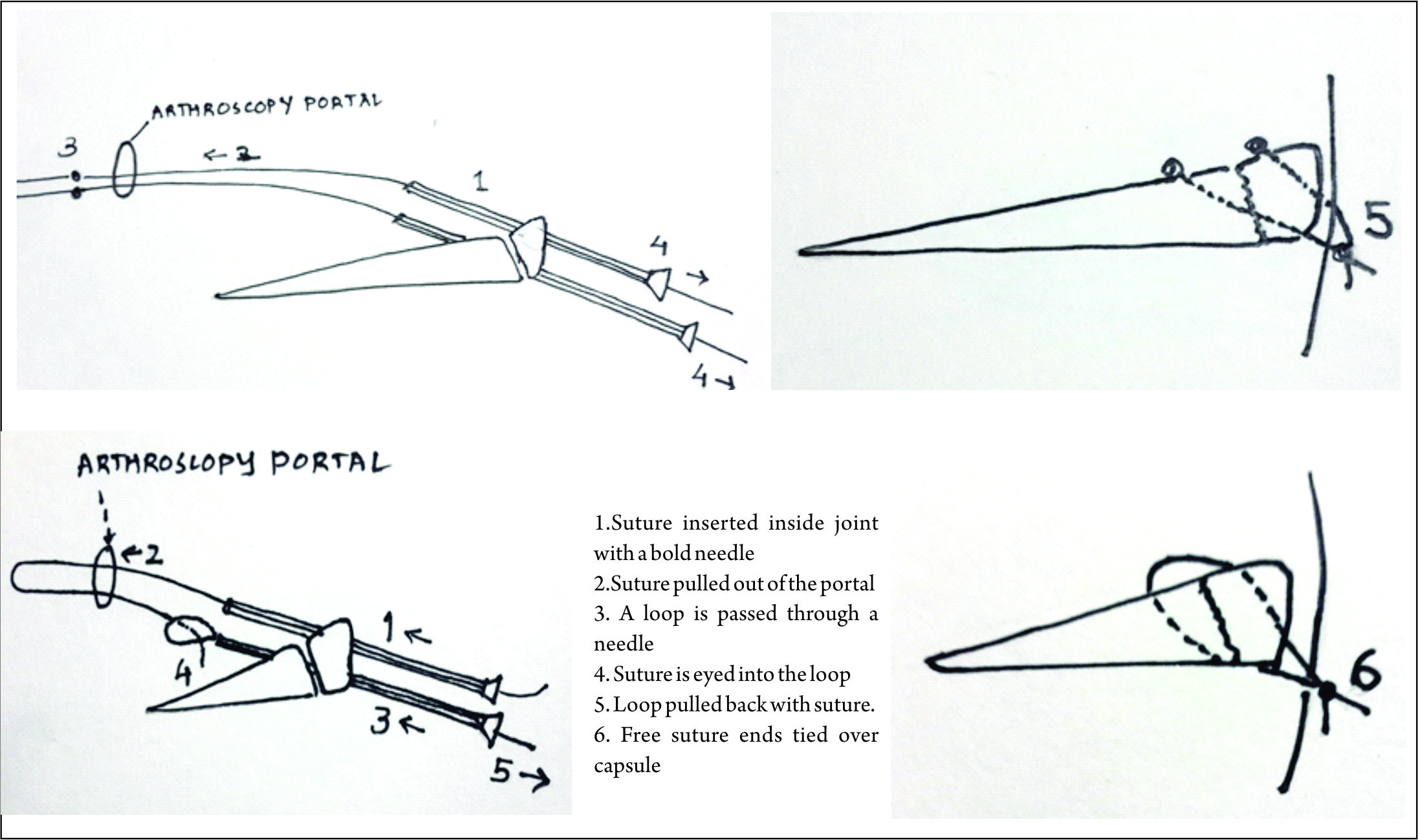
Many techniques for outside-in meniscus repair are proposed, each one following the same principle but tweaked by authors to make it either efficient or simpler. General preparation for meniscus repair includes high tourniquet, a leg stopper to keep the leg in 90 degree flexed position [3]. After painting and draping the leg, arthroscopy is performed to identify the site and type of the tear. Medial meniscus tear should be tackled in 10o degree flexion with valgus stress to tighten the capsule. Transillumination can be used to identify the saphenous vein and nerve before a needle is inserted, thus avoiding damage to those structures. Anterior horn tears are repaired in 60o to 90o of knee flexion and the needle insertion site is kept anterior to the pes anserinus to avoid saphenous nerve and vessels. Lateral meniscus tears are repaired in figure-of-4 position so that the peroneal nerve shifts posterior to the joint-line. Posterior horn tears of medial meniscus are best repaired when the needle is placed just posterior to pes anserinus tendons in 10-15o flexion, for lateral meniscus posterior horn tears the knee is kept in figure of 4 or 90o flexion. Abrading the torn surfaces of meniscal fragments with a meniscal rasp helps increase the healing potential. A needle is placed in the torn fragments, one in the femoral side and other in the tibial side in horizontal tears, piercing both fragments in a longitudinal tear and one in anterior and other in posterior part of a radial tear. The orientation of suture can be vertical mattress or horizontal mattress sutures depending upon the type of the tear and accessibility. Vertical mattress sutures have more pull-out strength as they are able to co-apt the circumferential fibres of the meniscus. Reduction and suturing of fragments have various techniques which have been described by many authors. One of the earliest of the techniques described was the Mulberry knot technique, where two separate non absorbable suture thread are passed in the superior and inferior portion of the torn meniscus using a bold needle. The sutures are pulled out from the anterior viewing portal, a mulberry knot is tied to each suture thread and then the sutures are pulled out along with the needles through which they were inserted thus reducing the meniscus tear. The free suture ends are then tied over the capsule from the point where they were inserted. Other technique is when a knot is tied with a few throws of simple suture to the 2 sutures outside the joint and then 1 end is pulled back in the joint with the knot piercing the meniscus and finally forming a loop suture around meniscus. A dilator knot which is a small sized knot may be tied preceding the big knot to help it pass through the meniscus and not tear it when it is pulled. The suture ends are tied over the capsule. A monofilament steel loop which is commercially available may be used to retrieve sutures as well. In this technique a loop is passed through the needles in the joint and the sutures are sewn into the loop hole from the portals using a grasper. The sutures are then retrieved over the capsule by retracting the loop. The procedure is repeated with other end of the same suture and the loop coming in through other fragment of the meniscus and the 2 free ends are tied on the capsule. A non-absorbable suture loop may be used instead of readymade loops. The progression of sutures is advised to be consistent in a way that superior and inferior fragments in a cleavage tear are reduced in sequence of superior first then inferior with repetition of the same sequence to have a uniform reduction of meniscus. Bucket handle tears are first stabilised by a central reduction sutures, followed by an anterior and a posterior sutures in sequence for uniform reduction. Many modified outside-in techniques have been described by various authors. Keyhani et al [4] have described a technique for vertical and horizontal loop sutures for anterior and middle third meniscus tears. A No. 0 PDS suture is passed through meniscus tibial end with a bold needle and the intra-articular end is retrieved through the joint. The procedure is repeated with other free end of the suture passed through femoral surface of meniscus and retrieved through same portal as the first suture end. A sliding knot is tied with few simple knots over the meniscus and the free ends are cut. Ahn et al [5] described a technique for reducing and repairing a free unstable end of anterior horn of the meniscus after decompression of cyst. They used a Linvatec hook, used for all inside suturing, to pierce the anterior free end of the horn using the loop from anterior portal. A suture is passed within the hook and the end is retrieved from the portal. With both the free ends now out from the same portal a loop is passed with a needle from capsule piercing the meniscus from outside -In. Loop is retrieved through same portal as sutures. The sutures are retrieved over the capsule by passing them from the loop and then retracting the loop and the needle. The suture ends are then tied over the capsule using a small stab incision.Yiannakopoulis et al [6] showed a simple technique where they used a spinal needle / suture hook to pierce longitudinal tears at first posteriorly, retiring the suture through portal. Keeping the same suture in the needle, the meniscus is pierced again a bit anterior-ly and the free end again retrieved through portal anteriorly. The free ends are tied with sliding knot over the meniscus giving a simple and effective configuration. Landsiedl [7] used needles to introduce two suture loops, one anterior and other a bit posterior to the first one. Both loops are retrieved outside the joint through portal and tied together and then one end is pulled gain bringing the knot inside the joint, the knot passing through the meniscus and thus forming a loop suture over the meniscus. The free ends are tied over the capsule. Chong et al [8] wrote about a technique where they passed a Loop through needle piercing both fragments of the meniscus and through the anterior portal introduced a reverse loop via needle with free ends inside the joint and loop end outside the joint . The free end is passed through the loop and loop is pulled with the suture. The process is repeated with the other free end of the reverse too and then when the 2 ends are re-trieved outside the joint they are tied over the capsule leaving no knot in the joint.
Complications
The technique of outside-in meniscus repair can be challenging and demanding. It may not always be possible to get the needles in right part of the meniscus or perpendicular to the tear in the first place. These techniques require a longer learning curve and patience to get sutures and needles placed in right spot. The outside-in technique has two stages which are critical. One is when a sharp pointed instrument is inserted in the joint and other while securing the suture by tying a knot over the capsule. Though techniques and landmarks are defined by many authors to avoid these injuries clinical practice not being perfect leads to these complications. Peroneal nerve injury is common if the knee is not placed in enough flexion and needle is inserted posterior while doing lateral meniscus repair. Saphenous nerve is at risk of injury during medial meniscus repairs. Posterior neurovascular structures are at risk of injury while performing Posterior horn medial meniscus (PHMM) repair. Hassad Sobhy [9] and colleagues carried out cadaveric dissections to evaluate the safety of outside-in meniscus techniques while performing PHMM repairs. They concluded that inserting a needle through a slit in the skin just over the semitendinosus has significant lower risk of damaging either popliteal vessels or saphenous nerve. Chondral damage during insertion of needles into the joint is a well-known complication. This can be avoided by carefully placing the needles and not thrusting them in. Intra-articular knots which are used to secure the repair in some techniques are also a cause of problems. Kelly IV and colleagues [10] carried out a second look arthroscopy in patients who had synovitis after meniscal repair with mulberry knot technique. They evaluated the prevalence of aseptic synovitis and evidence of chondral damage. The synovitis and clinical symptoms subsided after partial meniscectomy. Retears and healing problems are also part of the complications spectrum. Healing problems are most common in the posterior third of the meniscus since it is difficult to get the coaptation right due to improperly oriented needles. Posterior capsule tightness in a repair done in excessive flexion may also lead to extension loss.
Results
The results for outside in meniscus have been extremely promising. Out of the studies which have evaluated healing rates and outcome of meniscal repair, all of them have good healing rates with outside-in technique. This may be due to modularity that the surgeon has while placing the sutures. In a study by Morgan and Casscells [11] which evaluated clinically their patients who underwent outside-in repair for posterior horn tears, the authors reported 98% good to excellent clinical outcomes. The fallacy of this study was that it was only a clinical as-sessment. Morgan et al [12] did a study of 353 meniscus repairs done by outside-in technique. He performed second look arthroscopy on 74 of them at average 1 year post op and found out of the 84 % patients who had asymptomatic healing, 65 % had complete healing and 19% had incomplete healed meniscus. Interestingly all of the failures were in ACL deficient knees. They also concluded that it takes around 4 months to have visual evidence of healing.
Van Trommell et al [13] evaluated patients with outside-in repairs at a mean duration of 15 months by second look arthroscopy, arthrogram or MRI. They found 74% patients had complete or partial healing. All the Re-tears were in posterior and middle third of meniscus. Posterior third of meniscus is notorious for poor healing. They attributed improperly placed sutures for these failures. Mariani et al [14] gave accelerated rehabilitation to their patients of ACL reconstructions with outside-in meniscus repair and found 77% good to excellent results. All the new and modified techniques described above in techniques section also showed good to excellent clinical outcomes in their respective study at mid-term follow up. Hantes et al [15] published the only study available where they evaluated and compared outside-in, inside-out and all inside meniscus repair techniques. They clinically evaluated 57 patients who underwent meniscus repair. 17 out of 57 were in outside-in cohort and showed 100% clinical healing rate as compared to 95 % of Inside-out and 65% of All-inside cohort. Only one patient had saphenous palsy which resolved over 4 months, as compared to inside-out cohort which had four incidences of nerve palsy. The only downside attributed to outside-in cohort is longest surgical time as compared to other cohorts with and average surgical time of 38.5 minutes.
Conclusions
Outside-in meniscus repair have stood the test of time to be the most effective meniscus repair techniques. It provides surgeons the ability to modify the procedure to their liking and giving certain modularity helps in perfecting the suture placement techniques. This has resulted in better co-aptation of torn fragments leading to stable repairs and better healing rates. This is a demanding technique but has equally good proven results to make the steep learning curve worthwhile. The other advantage is less likelihood of complications if the identified landmarks and prescribed guidelines from previous studies are followed. The material and equipment required for the surgery is inexpensive and thus provides good cost-cutting in patient care without compromise in the results. New and modified Outside-in repair technique still have to be explored but the existing ones provide for repairing most of the tears giving equally good if not better outcomes than other techniques.
References
1.FairbankTJ.Kneejointchangesaftermeniscectomy.JBoneJointSurg1948;30B(4): 664 –70
2. Ikeuchi H. Trial and error in the development of instruments for endoscopic knee surgery. Orthop Clin North Am. 1982;13(2):255.
3. Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect. 2000;49:195-206.
4. Keyhani S, Abbasian MR, Siatiri N, Sarvi A, Kivi MM, Esmailiejah AA. Arthroscopic Meniscal Repair: “Modified Outside-In Technique”. Arch Bone Jt Surg. 2015 Apr;3(2):104-8.
5. Ahn JH, Wang JH, Yoo JC, Kim SK, Park JH, Park JW. The modified outside-in suture: vertical repair of the anterior horn of the meniscus after decompression of a large meniscal cyst. Knee Surg Sports Traumatol Arthrosc. 2006 Dec;14(12):1288-91. Epub 2006 Jul 5.
6. Yiannakopoulos CK, Chiotis I, Karabalis C, Babalis G, Karliaftis C, Antonogiannakis E. A simplified arthroscopic outside-in meniscus repair technique. Arthroscopy. 2004 Jul;20 Suppl 2:183-6.
7. Landsiedl F. Improved outside-in technique of arthroscopic meniscal suture. Arthroscopy. 1992;8(1):130-1.
8. Chong KC, Chan BK, Chang HC. A simple method of meniscus repair using the arthroscopic outside-in technique. Arthroscopy. 2006 Jul;22(7):794.e1-5.
9. Sobhy MH, AbouElsoud MM, Kamel EM, Desouki AM. Neurovascular safety and clinical outcome of outside-in repair of tears of the posterior horn of the medial meniscus. Arthroscopy. 2010 Dec;26(12):1648-54.
10. Kelly JD 4th, Ebrahimpour P. Chondral injury and synovitis after arthroscopic meniscal repair using an outside-in mulberry knot suture technique. Arthroscopy. 2004 May;20(5):e49-52.
11. Morgan CD, Casscells SW. Arthroscopic meniscus repair: a safe approach to the posteri-or horns. Arthroscopy 1986;2(1):3–12.
12. Morgan CD, Wojtys EM, Casscells CD, et al. Arthroscopic meniscal repair evalu- ated by second-look arthroscopy. Am J Sports Med 1991;19(6):632–7 [discus- sion: 637–8].
13. van Trommel MF, Simonian PT, Potter HG, Wickiewicz TL. Different regional healing rates with the outside-in technique for meniscal repair. Am J Sports Med.1998 May-Jun;26(3):446-52.
14. Mariani PP, Santori N, Adriani E, et al. Accelerated rehabilitation after arthroscopic me-niscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy 1996;12(6):680 – 6.
15. Hantes ME, Zachos VC, Varitimidis SE, Dailiana ZH, Karachalios T, Malizos KN. Arthroscopic meniscal repair: a comparative study between three different surgical techniques. Knee Surg Sports Traumatol Arthrosc. 2006 Dec;14(12):1232-7.Epub 2006 Jul 21.
16. Dave LY, Caborn DN. Outside-in meniscus repair: the last 25 years. Sports Med Arthrosc. 2012 Jun;20(2):77-85..
| How to Cite this article:. Tapasvi SR, Shekhar A. Outside -in Meniscus repair. Asian Journal of Arthroscopy. Aug – Nov 2016;1(2):19-22 . |