William M Weiss, F. Alan Barber
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 8-13
Author: William M Weiss[1], F. Alan Barber[2]
[1] Texas Tech University Health Sciences Center El Paso, Texas.
[2[ Plano Orthopedic Sports Medicine and Spine Center Plano, Texas.
Address of Correspondence
Dr William M Weiss
Texas Tech University Health Sciences Center Department of Orthopedic Surgery and Rehabilitation 4801 Alberta Avenue El Paso, Texas 79902.
E-mail: william.m.weiss@ttuhsc.edu
Abstract
Meniscal surgery has undergone a considerable shift in goals over the last century. While early meniscal surgery consisted of mostly total meniscectomy, recognition of the importance of this structure resulted in a shift to partial meniscectomy, and then to repair in appropriate patients. The over-reaching goal is now the preservation of meniscal tissue to minimize the risk of osteoarthritis, particularly in the young athlete. Technologic advances in arthroscopy and instrumentation have allowed the development of minimally invasive techniques, which decrease the risks associated with open surgery. While no meniscal repair technique has been demonstrated to be superior in its outcomes, the all-inside technique requires no accessory incisions and minimizes the risk to posterior structures. While the early all-inside implants have been shown to risk chondral damage, the literature demonstrates that newer suture-based implants do not share these complications, and result in the healing of appropriate tears.
Key Words: All-inside, Meniscal tear, Meniscal repair, Chondral injury.
Introduction
The first open meniscal repair was performed in 1885 [1], though resection has been more common. With the advent of arthroscopy, minimally invasive techniques replaced open repairs, and provided better access to difficult areas while minimizing surgical risks. The inside-out suture repair was initially the described, and continues to be used with excellent results [2]. The outside-in repair was developed later to decrease risk of injury to posterior neurovascular structures [3]. In recent years, advances in instrument and implant technology have allowed the development of all-inside repair techniques. These rely on specialized implants, but avoid additional incisions, decreasing risk to posterior neurovascular elements, and reducing surgical times [4]. The purpose of this review is to examine the evolution of the all-inside meniscal repair technique, with outcomes and complications.
Meniscus Anatomy, Function, And Healing:
The menisci are crescent shaped fibrocartilaginous structures situated in both the medial and lateral compartments of the knee, between the femur and tibia. Each meniscus has an anterior and posterior horn, and is attached to the tibia by the anterior and posterior meniscal roots and to the peripheral capsule by the coronary ligaments. They are triangular in cross section, conforming to both the distal femur and proximal tibia. This conformity effectively deepens the articular surfaces of the knee, providing shock absorption and contributing to stability, particularly with injury to stabilizing ligaments. This also increases the surface area for load distribution to the articular cartilage, decreasing contact stresses by converting vertical compression stresses to radially oriented hoop stresses [5, 6]. By maintaining space in the joint, the meniscus improves diffusion of synovial fluid, and provides nutrition and lubrication to the cartilage. The healing capacity of the meniscus is determined primarily by blood supply, as it is largely avascular and does not typically heal spontaneously. The meniscus is divided into zones in accordance with blood supply and healing capacity. The peripheral third (within 3 mm of the meniscosynovial junction) is well vascularized, as the blood supply enters the here [7]. This zone is referred to as red-red, and is mostly likely to heal. The inner third (over 5 mm from the meniscosynovial junction) receives no vascular supply, is called the white-white zone, and is least likely to heal. The middle zone, called red-white (between 3 to 5 mm from the meniscosynovial junction), has some vascularity [7, 8]. Red-red zone tears are commonly repaired in appropriate patients, while repairs of red-white zone tears are less likely to heal. Meniscal tear characteristics also influence healing potential. Longitudinal vertical tears (including bucket handle tears and meniscocapsular tears) have the capacity to heal with repair, while degenerative or complex (multi-planar), radial, horizontal, or flap tears are much less likely. Larger and less stable meniscal tears have higher failure rates, as have those repaired more than 8 weeks from injury [9]. Lateral compartment tears are also more likely to heal than those occurring medially [9]. This may be due to increased blood supply to the posterior horn of the lateral meniscus.
Meniscal Repair Technique
To overcome the inherent physiologic challenges of meniscal repair, the environment and technique must be optimized. Factors controlled by the surgeon include tissue preparation, the stability of fixation, knee stability and leg alignment, and post-operative rehabilitation. Preparation should include rasping of the tear, and the perimeniscal synovium. This stimulates the healing response [10], and can allow healing of isolated stable tears without fixation, particularly with concomitant ACL reconstruction [10,11]. Some advocate trephination to create vascular access channels, which may contribute to fibrovascular healing of avascular areas [12]. The addition of fibrin clot [13, 14], platelet-rich fibrin matrix [15], and collagen matrix with bone marrow [16] have been demonstrated to aid healing. Meniscal repair with associated ACL reconstruction improves healing, possibly by increasing blood in the joint, while lack of ACL function practically assures failure from stresses on the repair [17, 18]. ACL deficiency increased the failure rates of meniscal repair from 5% to 46% [19], demonstrating the importance of stability. Normal knee alignment also is required for successful meniscus repair outcomes. Forces within the knee, and through the meniscus, during normal gait can reach four times body weight and present significant challenges to fixation [20]. However, during unloaded knee motion the meniscus experiences only compressive forces [21, 22]. Therefore, fixation should maintain tissue approximation and neutralize sheer stresses. For suture-based repairs, vertically oriented non-absorbable sutures are considered the gold-standard, because of load to failure [23]. This configuration encircles the strong circumferential fibers, maximizing strength. Meniscus repairs are weak at the scar after 12 weeks 24, and visual evidence of healing at second-look arthroscopy has been seen at up to four months [25].
Surgical Technique Of Meniscus Fixation:
Arthroscopic techniques are the preferred method for meniscal repair; however no consensus exists as to the best technique. The most common indication for all-inside repair is tears of the posterior horn, as risk to neurovascular structures is decreased. All-inside repairs require less surgical time than other methods [26]. However, all-inside repairs do require an intact meniscal rim, highly specialized instruments, and implants. All-inside meniscal repair devices have progressed from rigid implants to current adjustable suture-based devices. Earlier versions of all-inside devices are no longer widely used or recommended. The adjustable suture-based all-inside devices are the state of the art.
Self-Adjusting Suture Containing Implants
The current generation of all-inside devices use ultra-high molecular weight polyethylene (UHMWPE) containing suture to connect typically non-absorbable poly ether-ether-ketone (PEEK) anchors. The suture is pre-tied, typically with a sliding and self-locking knot. Insertion instruments require only standard anterior portals, and often use a disposable cannula or a skid to aid passage. The meniscus repair device is inserted through the inner meniscus fragment to a pre-determined depth of the peripheral rim, often guided by the cannula. Once both anchors are deployed, the sliding-locking knot is cinched to compress the tear. This adjustability allows appropriate tensioning for reduction and healing, and the option to place horizontal, oblique, or vertical configurations.
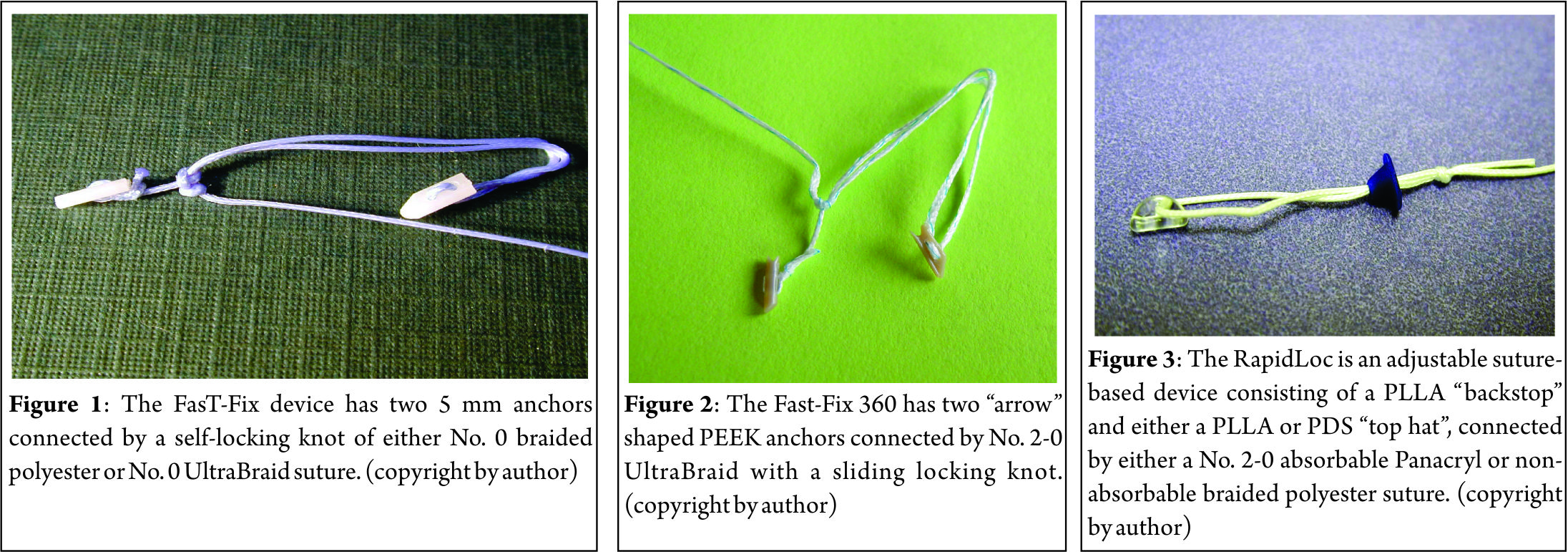
The FasT-Fix (Smith & Nephew, Andover, MA) was the first adjustable suture-based device (Fig. 1). It consisted of two 5 mm anchors, made of either poly L lactic acid (PLLA, absorbable) or polyacetal (nonabsorbable) connected by No. 0 non-absorbable braided polyester suture. The anchors are delivered by an instrument that is either straight or angled 22°. Once both anchors span the tear, the pre-tied sliding-locking knot is tensioned using a knot pusher/suture cutter. The original design was modified to become the Ultra Fast-Fix by reconfiguring the needle to facilitate insertion, and replacing the suture with a stronger No. 0 UHMWPE UltraBraid. The current iteration is the FasT-Fix 360 (Fig. 2), in which the anchors have been reconfigured to PEEK with an arrow design, and the suture is now No. 2-0 UltraBraid.
The RapidLoc (Mitek, Raynham, MA) was an adjustable suture-based device, consisting of a PLLA “backstop” and a PLLA or polydioxanone (PDS) “top hat”, connected by either a No. 2-0 absorbable Panacryl or non-absorbable braided polyester suture (Fig. 3). The “backstop” anchor was placed across the tear to be extra-capsular, and the pre-tied sliding knot and “top hat” was then advanced, compressing the tear. The instrument included straight, 12° and 27° angled needles.
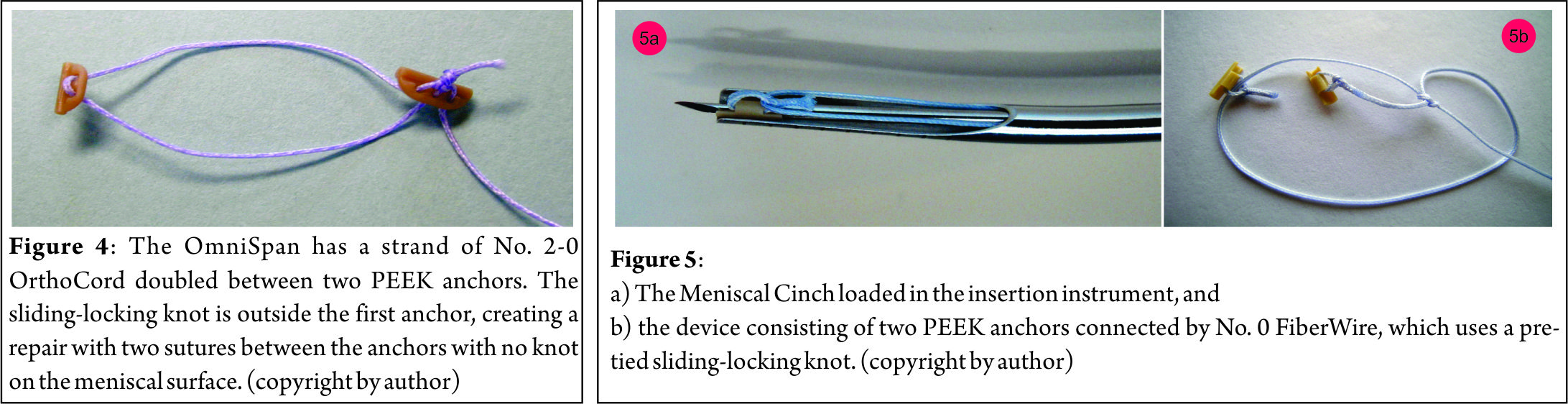
The OmniSpan (Mitek, Raynham, MA) replaced the RapidLoc, and uses a loop of No. 0 OrthoCord (55% PDS and 45% UHMWPE) suture between two PEEK anchors (Fig. 4). The sliding-locking knot is outside the loop, reinforcing the first anchor, and forming a double suture repair without a knot on the articular surface. Both loops of the repair are tightened concurrently, allowing equal tension. This device allows sutures to be placed in both horizontal and vertical mattress fashion.
The Meniscal Cinch (Arthrex, Naples, FL) has undergone incremental improvements since its inception (Fig. 5). The device is inserted with a 15° curved “gun” containing two separate trocar needles. It has an adjustable depth limiter on the handle, which is most commonly used at 18 mm. Each needle is loaded with a tubular PEEK anchor, and connected with a No. 2-0 FiberWire composed of UHMWPE and braided polyester (Arthrex Inc, Naples FL). The system includes a blue plastic “shoehorn” cannula to facilitate insertion, which is 6 mm in diameter and requires a large portal. The instrument allows placement of a vertical mattress stitch, secured with a pre-tied sliding-locking knot. After insertion, the first needle is removed and handed off. The second needle is “clicked” into position, and then a second device is inserted. Once both devices are deployed, the suture is gently pulled at the handle to tension the repair. A disposable knot pusher/suture cutter is provided.
The Sequent meniscal repair device (ConMed Linvatec, Largo, FL) utilizes No. 0 Hi-Fi (braided UHMWPE) suture with up to seven PEEK anchors measuring 1.3 mm in diameter and 5.1 mm long (Fig. 6). Each anchor is placed individually through the meniscus, with a straight or 15° curved instrument, and deployed on the extra-capsular surface. The suture is then tensioned to set the anchor into the tissue, and additional anchors can then be placed with the same device. A minimum of 3 anchors must be inserted to complete the repair, although more can be used to create an all-inside continuous stitch. This allows numerous stitch configurations, from continuous to interrupted stitches, and vertical or horizontal mattresses. This is the only device that can place multiple stitches without removal from within the joint. However, the technique is demanding, and practice in the laboratory prior to use is advised. The set includes a side-loading disposable suture cutter for use at completion.
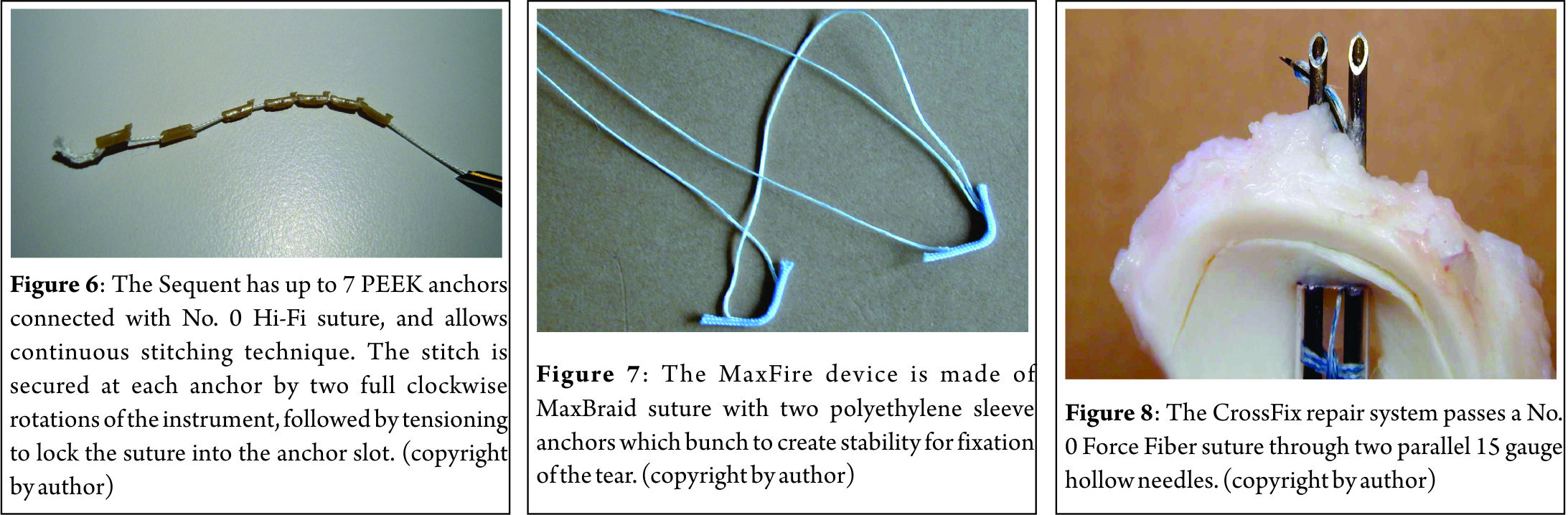
The MaxFire MarXmen (Biomet Sports Medicine, Warsaw, Indiana) is an self-adjusting all-inside all-suture implant with No. 0 MaxBraid PE (UHMWPE) and two braided polyester sleeves serving as anchors (Fig. 7). It is similar to the JuggerKnot all-suture anchor in design and function, but modified for the meniscus. The instrument uses a needle (straight or curved) to insert the suture and two polyester anchors through the meniscus. The sliding-locking knot allows tensioning, and devices can be placed in either a horizontal or vertical mattress fashion.
The CrossFix meniscal repair system (Cayenne Medical, Scottsdale, AZ) passes a No. 0 Force Fiber (UHMWPE) suture through two parallel 15 gauge hollow needles (straight or curved 12°, Fig. 8). Once the needles penetrate the meniscus, crossing the tear, a small shuttle passes the suture from one needle to the other on the extra-capsular surface. As the needles are withdrawn, a 3 mm horizontal mattress suture is left, and a pre-tied sliding Weston knot is advanced to secure the reduction. Additional arthroscopic knots can be added as reinforcement, if desired.
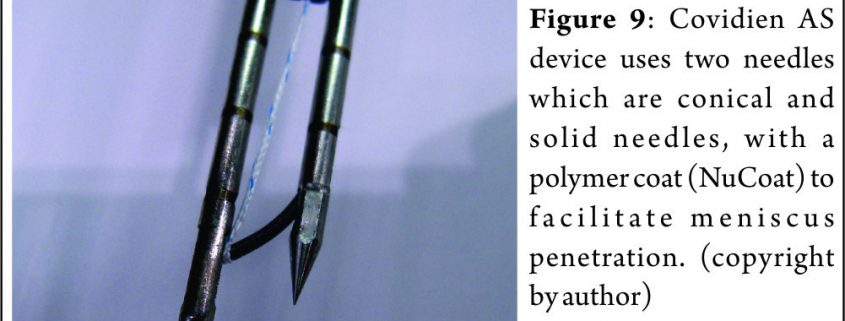
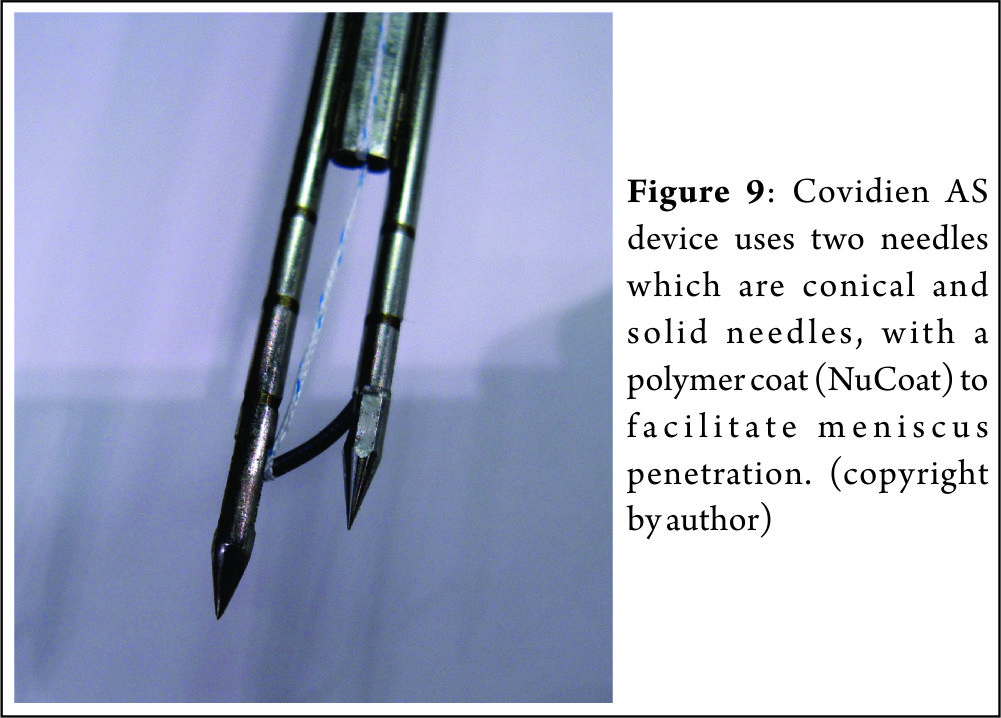
The AS (all suture) Repair device (Covidien, Minneapolis, MN) is similar to the CrossFix in design and function (Fig. 9). While the two needles are the same size, the AS repair device has conical solid needles with a polymer coat (NuCoat) to facilitate penetration. The instrument can be straight or curved 15°, and passes a No. 2-0 UHMWPE suture using a similar shuttle needle, but uses a modified Tennessee slider knot with two half hitches to secure the repair. Both instruments result in a 3 mm wide horizontal mattress, with a knot on the meniscal surface that risks chondral injury. Due to the instrument dimensions, only horizontal mattress sutures are possible. Conceptually, this newest generation of all-inside suture based devices allows improved reduction, tissue compression, and stability compared to previous iterations. The overall goal of all-inside meniscal repair devices is to decrease complications seen with the earlier generations, and promote healing. However, these devices can generate significant tension which may be detrimental, leading to implant failure. Few investigations regarding outcomes and complications of these adjustable all-inside suture implants are available in the literature.
Results Of All-inside Meniscal Repair:
Arthroscopic meniscal repair methods have similar outcomes to open methods, with the gold standard inside-out suture repair having a success rate of 82% [17, 27], and outside-in suture repairs having success rates as high as 87% [28]. The original suture-based all-inside technique described by Morgan reported good results, but without any long term follow-up [29]. Early devices which rely on arthroscopic knot tying demonstrate up to 90% success initially, but this declines to 81% at 1 year [30].
Suture based implants have good strength, and are biomechanically equivalent to the gold standard vertical mattress sutures [31,32]. However, as this is the latest generation of all-inside devices, there is little long term outcome data available. The RapidLoc has demonstrated success rates of 86 to 91% [33, 34, 35], but there are reported failure rates of 35% [36] with complications reminiscent of rigid devices [37]. Longer term follow-up of these devices shows re-operation rates of 48% [38]. The FasT-Fix has also shown success rates from 82 to 92% [39,40], but with limited reports of complications. All-Inside devices have been demonstrated to have greater failure strength than inside out alternatives in the repair of radial meniscal tears [41].
Comparison Of Meniscal Repair Devices: Author’s preferred technique:
A human cadaver knee based comparison of several all-inside meniscus repair devices was carried out by the senior author to compare the technical ease, reproducibility, and consistency of using these devices in human meniscus tissue. A needle penetration depth limited to 18mm was found to be anatomically safe. Curved needles effectively reached the posterior horn with minimal articular cartilage injury. However, significant differences were observed in the technical ease, reproducibility, and consistency of all these devices. The FastFix 360 and OmniSpan were easiest to insert, least likely to excoriate articular cartilage, and most consistent in performance. Yet, the OmniSpan did not have any knot or device on the surface to later damage the articular cartilage. Based upon this data the author’s preferred technique uses the OmniSpan. The control provided by the gun allows for better positioning of the implants and decreased articular cartilage damage. Prototypes of the next generation of OmniSpan (the TrueSpan) perform even better but await clinical experience to confirm our expectations of superior performance.
Complications
All-inside meniscus repair has all the known risks and potential complications of knee arthroscopy. These occur in approximately 1% of patients, and include neurovascular injury, infection, and thrombophlebitis [42]. While neurovascular injuries are likely the most common complication of knee arthroscopy, when compared to other meniscal repair techniques the risk of this complication with all-inside repairs is decreased. Neurologic injury rates as low as 2% have been reported for all-inside techniques, in comparison to 9% for inside-out repairs [43]. The development of the all-inside technique was primarily to eliminate the need for accessory incisions and suture passing that are responsible for most of the neurovascular risk, so that repairs in the posterior horn can be done more safely. Injury to the saphenous nerve is most frequent, but as it is a sensory nerve this is often of little consequence [44]. Peroneal nerve palsy and popliteal artery pseudoaneurysm have also been reported 45, as have cases of cyst formation and synovitis [46, 47]. Complications associated with the adjustable-suture based current generation of all-inside devices include over penetration of the implant, loss of fixation, inadequate tension, and problems with implant deployment [48,49]. An overall complication rate for all-inside repair of 19% has been reported comparable to the gold standard [43]. The RapidLoc has caused cartilage injury in limited reports [50,37], and cadaveric studies have demonstrated placement of these implants may be challenging, but the significance of this is unclear [48,49]. Complications of all-inside repair can be minimized with detailed knowledge of anatomy, proper portal placement, measurement of meniscal depth, and placement of the indicated implant in an appropriate and secure manner.
Rehabilitation:
Post-operative rehabilitation following meniscus repair is highly variable between surgeons, with little consensus in the literature. Early knee motion is thought to be advantageous, as prolonged immobilization is known to lead to stiffness, atrophy, and impaired healing of the meniscus [51]. However, higher degrees of knee flexion cause considerable posterior translation of the femoral condyles, which increases forces within the meniscus and may stress repairs [52]. Weight-bearing can help reduce and stabilize longitudinal (bucket-handle) meniscus tears due to radially directed hoop-stresses [22], but loads with knee flexion cause increasing shear forces in the meniscus. These forces are increased almost four times with the combination of weight-bearing and flexion to 90 degrees [52]. Based on this information, weight-bearing in full extension poses little risk to repairs of longitudinal meniscal tears, and may aid with reduction and healing. However, for radial or meniscal root tear repairs (which are challenging with limited success), weight bearing is not advisable since circumferential fibers are not intact and the tear will be distracted. Accelerated rehabilitation programs designed to return patients to sport earlier have been described [53, 54], permitting early full weight bearing and unrestricted knee motion. The only limitations on return to sport in accelerated programs are the resolution of postoperative effusion, and return of full motion. Thus far, results of accelerated programs have shown return to sport without re-injury or complications. Meniscal repair in the setting of ACL reconstruction presents unique challenges. There is no evidence to support slowing ACL rehabilitation for an associated meniscal repair, and with the increased stability of new adjustable suture-based devices there is less reason to do so 55. The author’s current protocol for modern all-inside devices allows immediate range of motion from 0 to 90 degrees, immediate full weight bearing, early closed-chain strengthening, flexibility and endurance training. After 2 months, full flexion is allowed, and full return sport is permitted once the knee has no effusion, has regained full extension, and demonstrates flexion to greater than 135°.
Conclusions
Advances in arthroscopy and instrumentation technology have made all-inside meniscal repair popular and effective in appropriate meniscal tears. While no arthroscopic method has proven to have superior outcomes in the literature, all-inside methods are indicated for posterior horn meniscal tears to minimize the risk to neurovascular structures. The adjustable suture-based designs have so far demonstrated improved versatility and outcomes comparable to other methods. The versatility of these implants also allows their use in meniscal repairs that are not repairable by other methods, promoting the preservation of meniscal tissue when possible.
References
1. Annandale T. An operation for displaced semilunar cartilage. Br Med J 1885;1:779.
2. Henning CE. Arthroscopic repair of meniscus tears. Orthopedics 1983;6:1130-2.
3. Warren RF. Arthroscopic meniscus repair. Arthroscopy 1985;1:170-2.
4. Ahn JH, Yoo JC, Lee SH. Posterior horn tears: all-inside suture repair. Clin Sports Med;31:113-34.
5. Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res 1980;149:283-90.
6. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med 1986;14:270-5.
7. Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-5.
8. Arnoczky SP, Warren RF. The microvasculature of the meniscus and its response to injury. An experimental study in the dog. Am J Sports Med 1983;11:131-41.
9. Cannon WD, Jr. Arthroscopic meniscal repair. Inside-out technique and results. Am J Knee Surg 1996;9:137-43.
10. Okuda K, Ochi M, Shu N, Uchio Y. Meniscal rasping for repair of meniscal tear in the avascular zone. Arthroscopy 1999;15:281-6.
11. Fitzgibbons RE, Shelbourne KD. “Aggressive” nontreatment of lateral meniscal tears seen during anterior cruciate ligament reconstruction. Am J Sports Med 1995;23:156-9.
12. Zhang Z, Arnold JA, Williams T, McCann B. Repairs by trephination and suturing of longitudinal injuries in the avascular area of the meniscus in goats. Am J Sports Med 1995;23:35-41.
13. Arnoczky SP, Warren RF, Spivak JM. Meniscal repair using an exogenous fibrin clot. An experimental study in dogs. J Bone Joint Surg Am 1988;70:1209-17.
14. Henning CE, Lynch MA, Yearout KM, et al. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res 1990;252:64-72.
15. Sgaglione NA. Meniscus repair update: current concepts and new techniques. Orthopedics 2005;28:280-6.
16. Piontek T, Ciemniewska-Gorzela K, Naczk J, et al. Complex Meniscus Tears Treated with Collagen Matrix Wrapping and Bone Marrow Blood Injection: A 2-Year Clinical Follow-Up. Cartilage 2016;7:123-39.
17. Cannon WD, Jr., Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med 1992;20:176-81.
18. Hanks GA, Gause TM, Handal JA, Kalenak A. Meniscus repair in the anterior cruciate deficient knee. Am J Sports Med 1990;18:606-611.
19. Schmitz MA, Rouse LM, Jr., DeHaven KE. The management of meniscal tears in the ACL-deficient knee. Clin Sports Med 1996;15:573-93.
20. Morrison JB. Function of the knee joint in various activities. Biomed Eng 1969;4:573-80.
21. Richards DP, Barber FA, Herbert MA. Meniscal tear biomechanics: loads across meniscal tears in human cadaveric knees. Orthopedics 2008;31:347-50.
22. Richards DP, Barber FA, Herbert MA. Compressive loads in longitudinal lateral meniscus tears: a biomechanical study in porcine knees. Arthroscopy 2005;21:1452-6.
23. Starke C, Kopf S, Petersen W, Becker R. Meniscal repair. Arthroscopy 2009;25:1033-44.
24. Roeddecker K, Muennich U, Nagelschmidt M. Meniscal healing: a biomechanical study. J Surg Res 1994;56:20-27.
25. Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med 1991;19:632-637.
26. Barber FA, Coons DA. Midterm results of meniscal repair using the BioStinger meniscal repair device. Arthroscopy 2006;22:400-405.
27. Johnson D, Weiss WM. Meniscal repair using the inside-out suture technique. Clin Sports Med 2012;31:15-31.
28. Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect 2000;49:195-206.
29. Morgan CD. The “all-inside” meniscus repair. Arthroscopy 1991;7:120-5.
30. Barrett GR, Treacy SH, Ruff CG. Preliminary results of the T-fix endoscopic meniscus repair technique in an anterior cruciate ligament reconstruction population. Arthroscopy 1997;13:218-23.
31. Borden P, Nyland J, Caborn DN, Pienkowski D. Biomechanical comparison of the FasT-Fix meniscal repair suture system with vertical mattress sutures and meniscus arrows. Am J Sports Med 2003;31:374-8.
32. Barber FA, Herbert MA, Richards DP. Load to failure testing of new meniscal repair devices. Arthroscopy 2004;20:45-50.
33. Quinby JS, Golish SR, Hart JA, Diduch DR. All-inside meniscal repair using a new flexible, tensionable device. Am J Sports Med 2006;34:1281-6.
34. Billante MJ, Diduch DR, Lunardini DJ, et al. Meniscal repair using an all-inside, rapidly absorbing, tensionable device. Arthroscopy 2008;24:779-85.
35. Barber FA, Coons DA, Ruiz-Suarez M. Meniscal repair with the RapidLoc meniscal repair device. Arthroscopy 2006;22:962-6.
36. Hantes ME, Zachos VC, Varitimidis SE, et al. Arthroscopic meniscal repair: a comparative study between three different surgical techniques. Knee Surg Sports Traumatol Arthrosc 2006;14:1232-7.
37. Barber FA. Chondral injury after meniscal repair with rapidLoc. J Knee Surg 2005;18:285-8.
38. Solheim E, Hegna J, Inderhaug E. Long-term outcome after all-inside meniscal repair using the RapidLoc system. Knee Surg Sports Traumatol Arthrosc 2016;24:1495-500.
39. Kalliakmanis A, Zourntos S, Bousgas D, Nikolaou P. Comparison of arthroscopic meniscal repair results using 3 different meniscal repair devices in anterior cruciate ligament reconstruction patients. Arthroscopy 2008;24:810-6.
40. Barber FA, Schroeder FA, Oro FB, Beavis RC. FasT-Fix meniscal repair: mid-term results. Arthroscopy 2008;24:1342-8.
41. Branch EA, Milchteim C, Aspey BS, et al. Biomechanical comparison of arthroscopic repair constructs for radial tears of the meniscus. Am J Sports Med 2015;43:2270-6.
42. Small NC. Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy 1988;4:215-21.
43. Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med 2012;40:459-68.
44. Austin KS. Complications of arthroscopic meniscal repair. Clin Sports Med 1996;15:613-619.
45. Brasseur P, Sukkarieh F. [Iatrogenic pseudo-aneurysm of the popliteal artery. Complication of arthroscopic meniscectomy. Apropos of a case]. J Radiol 1990;71:301-4.
46. Choi NH, Kim SJ. Meniscal cyst formation after inside-out meniscal repair. Arthroscopy 2004;20:E1-3.
47. Kelly JDt, Ebrahimpour P. Chondral injury and synovitis after arthroscopic meniscal repair using an outside-in mulberry knot suture technique. Arthroscopy 2004;20:e49-52.
48. Miller MD, Blessey PB, Chhabra A, Kline AJ, Diduch DR. Meniscal repair with the Rapid Loc device: a cadaveric study. J Knee Surg 2003;16:79-82.
49. Miller MD, Kline AJ, Gonzales J, Beach WR. Pitfalls associated with FasT-Fix meniscal repair. Arthroscopy 2002;18:939-43.
50. Cohen SB, Anderson MW, Miller MD. Chondral injury after arthroscopic meniscal repair using bioabsorbable Mitek Rapidloc meniscal fixation. Arthroscopy 2003;19:E24-6.
51. Dowdy PA, Miniaci A, Arnoczky SP, Fowler PJ, Boughner DR. The effect of cast immobilization on meniscal healing. An experimental study in the dog. Am J Sports Med 1995;23:721-8.
52. Becker R, Wirz D, Wolf C, et al. Measurement of meniscofemoral contact pressure after repair of bucket-handle tears with biodegradable implants. Arch Orthop Trauma Surg 2005;125:254-60.
53. Barber FA. Accelerated rehabilitation for meniscus repairs. Arthroscopy 1994;10:206-10.
54. Mariani PP, Santori N, Adriani E, Mastantuono M. Accelerated rehabilitation after arthroscopic meniscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy 1996;12:680-6.
55. Barber FA, Click SD. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy 1997;13:433-7.
| How to Cite this article:. Weiss WM, Barber FA. All-Inside Meniscus Repair. Asian Journal of Arthroscopy Aug – Nov 2016;1(2):8-13. |