Meniscectomy-Outcomes and Complications
Shantanu Sudhakar Patil, Sachin Ramchandra Tapasvi, Anshu Shekhar
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 53-55.
Author: Shantanu Sudhakar Patil[1], Sachin Ramchandra Tapasvi[1], Anshu Shekhar[1].
[1] The Orthopaedic Speciality Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004.
Address of Correspondence
Dr Sachin Ramchandra Tapasvi
The Orthopaedic Speciality Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004
Email: stapasvi@gmail.com
Abstract
The menisci, once considered expendable remnants have been conclusively proven to be of extreme vitality in the biomechanics and biology of the knee joint. Though meniscus repair is being increasingly performed to preserve knee function, not all tears are amenable to repair and partial meniscectomy in such cases is an acceptable treatment option. The poor outcomes following partial meniscectomy are due to the shrinking of contact areas and rise in peak stresses. These changes and their consequences are more pronounced in the lateral compartment of the knee. Pre-existing chondral damage, instability and higher BMI compound the problem.
Key words: Meniscus, meniscectomy, meniscus repair, arthritis.
Introduction
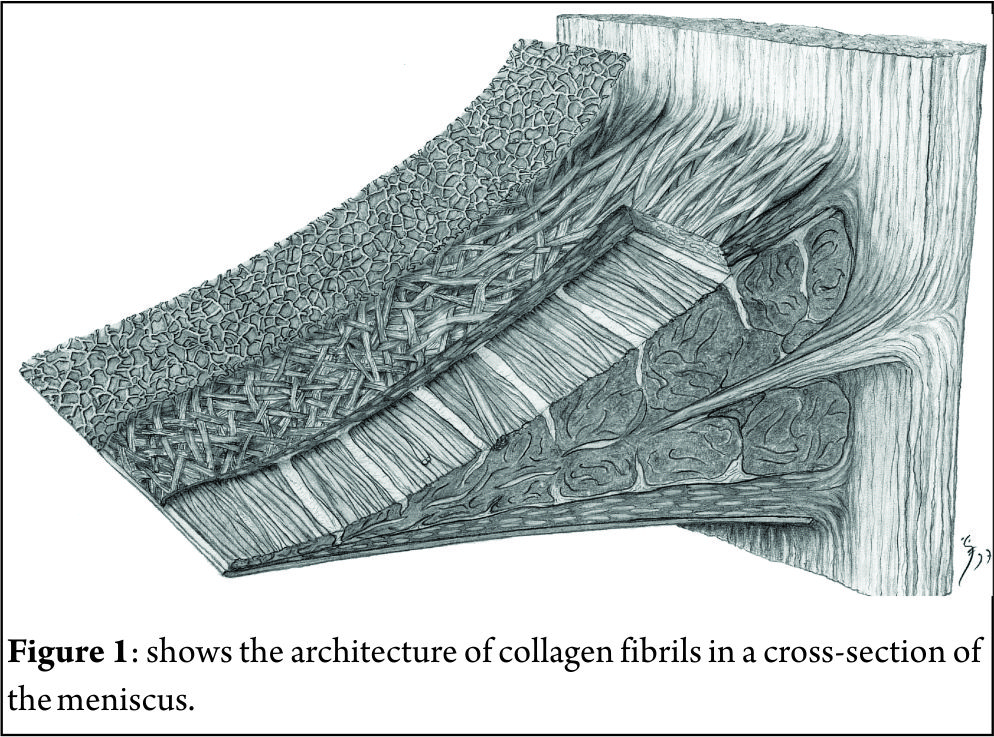
The menisci of the knee joint are fibrocartilagenous semilunar tissues that perform a critical function of stabilising the joint and aiding in efficient load transfer as a shock absorber. Though once considered vestigial and hence disposable, the role of healthy menisci in delaying the normal attrition of the articular cartilage cannot be understated. Meniscectomy was thought to be a benign procedure and as late as 1975 [1] the importance of doing a complete removal was being reiterated. The functions of the meniscus were recognised much earlier [2] and eventually the potential harms of its excision were gaining attention. Meniscal tears are one of the commonest injuries of the knee, for which treatment is sought, with an incidence rate of 61 per 100000 population per year.[3] Most acute tears are commoner in younger patients, with the medial meniscus affected at a 2:1 ratio with the lateral side. The acute tears are described as per their orientation and extent along the meniscus. They are usually classified as vertical longitudinal, oblique, circumferential, complex, transverse or radial, and horizontal cleavage tears. Radial tears of the posteromedial compartment are the most frequently seen tears and vertical longitudinal tears are most often associated with acute ACL injury. Degenerative tears have a varied pattern and are complex in their morphology.[4]. The direction of the meniscus tears is explained by the orientation of collagen fibrils within the structure. The cross section of the meniscus reveals three distinct layers: a superficial thin layer on both tibial and femoral surfaces; a lamellar layer below this with the fibrils arranged in a radial manner and a main central region where the fibrils are orientated in a circular manner. The circular arrangement of the collagen bundles explains why majority of the tears have a longitudinal orientation. [5](Fig. 1). With our growing understanding of the anatomy , vasculature, biomechanics and the biology of the meniscus, and with improved arthroscopic techniques and instrumentation, the goal of management of meniscal tears has shifted towards achieving repair. However, not all tears are amenable to repair and at least a partial meniscectomy might be indicated to alleviate the patients symptoms. We will take a look at the outcomes and complications of arthroscopic meniscectomy in this article.
Sequelae of articular cartilage changes following Meniscectomy
The effects of meniscectomy on the stability and pressures inside the knee joint were studied using pressure sensitive films in cadavers. Medial meniscectomy caused the contact areas to shrink by almost 75% leading to more than twofold increase in peak contact pressures. [6] The articular cartilage responds unfavourably to the higher loads, with disruption of the proteoglycan matrix, causing swelling and inflammation throughout the joint. The heightened catabolic state with increased hydration leads to breakdown of the collagen matrix, thus accelerating the normal wear and tear within the joint.[7]
Radiological changes:
The radiological changes in the knee joint following medial meniscectomy are well documented.[8]Joint space narrowing, flattening of the marginal part of the medial femoral condyle and sclerosis of the articulating condyles is seen. These radiological signs were indicative of early osteoarthritic changes in the knee. Multiple clinical and radiological studies have documented these sequelae, but the correlation between the symptoms of the patient and severity of these changes is not always seen in the results. It is not easy to determine the correlations as many reports have studied the consequences after an open meniscectomy. Moreover, a meniscal tear rarely presents in isolation and the concomitant ligament or articular injuries play a role in subsequent degeneration and development of Osteoarthritis.
Partial Versus Total meniscectomy
With the advent of arthroscopic surgery and advances in instrumentation for the various surgical procedures, it was possible to resect only the offending parts of the torn meniscus. It is uncommon these days to perform a total resection, with partial meniscectomy being the more widely reported procedure. Once a meniscal tear is identified and deemed unsuitable for repair, a meniscectomy is the recommended surgical option. The basic principles for this were described by Metcalf. They are as follows: Remove all mobile fragments; Avoid sudden changes in rim contour; a perfectly smooth rim is unnecessary as some remodelling may occur; re-evaluate the tear often with a probe; Avoid damage to the meniscus-capsular junction to avoid the loss of hoop stresses; Use both manual and motorized instruments to maximize efficiency and when uncertain if an area should be resected, err on the side of leaving more meniscus intact rather than compromising biomechanical properties[9]. Salata in a meta-analysis showed the significantly higher risk of developing radiographic OA in the patients undergoing total meniscectomy as compared to the partial meniscectomy. [10] Though the patients with either partial or total meniscectomy report similar early clinical results, there was no significant difference in the radiographic outcomes at the final 7.8 years average follow-up[11]. Only 68% of the patients who had undergone a total meniscectomy and followed up for up to 30 years showed good or excellent results while at least 2/3rd had some post-operative symptoms.[12] There exists a direct correlation with the meniscal tissue left behind and peak contact stress on the tibial surfaces following partial resections[13]. A finite element study quantifying the amount of resected meniscus to peak pressures showed that with as little as 20% resection of meniscus, a detrimental increase of forces is seen which may hasten the osteoarthritic changes. Maximum shear stress in the articular cartilage is seen with 65% partial meniscectomy[14]. The orientation of collagen fibril bundles within the meniscus determines the development of hoop strains as they are axially loaded. A radial tear disrupts the continuity of the circularly oriented fibrils and thus prevents the hoop strains from forming, causing dysfunction of the meniscus. A horizontal or vertical tear will not disrupt this continuity, preserving the load-bearing and shock-bearing function of the meniscus.[15] This needs to be borne in mind while determining the extent of the meniscectomy. The medial and lateral tibio-femoral articulations are anatomically different and the absence of menisci which afford a degree of congruity can lead to increased point loading and higher contact pressures. This is more prominent on the lateral side where a convex lateral femoral condyle articulates on a flat or convex tibial plateau. This translates to poorer outcomes with lateral meniscectomy as compared to medial as reported in multiple studies. Patients with a lateral meniscectomy have a much higher functional deterioration and increased instability than the medial meniscectomy patients[11,3,16].
Influence of other concomitant factors
The ACL-deficient knee with a meniscal tear has a significantly higher radiographic grade changes after meniscectomy as compared with ACL-intact knees.[17] Consequences of meniscectomy in an unstable knee are worsened by the combination of higher contact forces inducing early pathological changes due to the elevated shear stresses within the articular cartilage.[18] The presence of pre-existing chondral damage at the time of meniscectomy predisposes the knee to a significant increase in development of OA leading to poor clinical outcomes. However, contradicting findings have also been reported with there being no significant changes in knee functions and activity level following the meniscectomy. [19]. Chondral lesions can cause similar symptoms as that of a meniscal tear and meniscectomy may not fully alleviate the patients’ complaints, thus leading to poor outcomes. Degenerative tears are more often seen in older subjects with varus alignment. However, the evidence that meniscectomy in this group leads to higher rate of radiographic OA is not conclusive. These patients do show a decreased level of activity along with poorer outcomes based on subjective and functional measures following the surgery.[19, 20]While there is consensus about patients with increased BMI predisposing to a higher risk of OA post meniscectomy, the exact level of BMI that placed the patient at risk is not conclusive.[11], [21].
Complications
These can be classified as those related to knee arthroscopy in general and those associated specifically with arthroscopic partial meniscectomy. In the hands of an experienced arthroscopy surgeon, the complication rates were low. (1.78% and 1.48% for medial and lateral meniscectomy) [22], [23]. Some of the enumerated complications include instrument failure or breakage, injuries to nerves and blood vessels, accidental damage to chondral surfaces and ligament injury. Instrument failure rates have dropped from 18.1% to 2.9% over the years, due to improvement in surgical techniques, better designs as well as better skill levels of the surgeons[22]. The medial collateral ligament may get injured due to excessive valgus forces while attempting access to the medial compartment. Similarly, nerves and vessels may get damaged during insertion of sharp instruments. Improper and clumsy handling of instruments during the surgery can gouge the articular surface causing damage. Incomplete removal of the torn pieces can cause persistent pain along with coexistent knee pathology. Proper adherence to basic principles of partial meniscectomy can help avoid all these complications.
Conclusion
There exist a large number of studies which have studied the consequences of meniscectomy as a surgical procedure. Many of these have incomplete or inaccurate information along with varying heterogeneous criteria for evaluation of outcomes. The functional and clinical outcomes do not necessarily match the radiological outcomes in most of the studies. The multiple imaging modalities add to data which is not uniform for evaluation. This lack of homogenous data and lack of standardization of methodological issues, makes it difficult to conclude if the findings represent true differences or are simply artefact related to measurement bias or other errors. It is probably safe to conclude that a minimally invasive procedure with attention to sparing bulk of meniscal tissue seems to reduce the subsequent incidence of arthritic changes, as compared with open invasive and radical procedures..
References
1. Hughston, J.C., A simple meniscectomy. J Sports Med, 1975. 3(4): p. 179-87.
2. King, D., The healing of semilunar cartilages. 1936. Clin Orthop Relat Res, 1990(252): p. 4-7.
3. Jones, J.C., et al., Incidence and risk factors associated with meniscal injuries among active-duty US military service members. J Athl Train, 2012. 47(1): p. 67-73.
4. Pauli, C., et al., Macroscopic and histopathologic analysis of human knee menisci in aging and osteoarthritis. Osteoarthritis Cartilage, 2011. 19(9): p. 1132-41.
5. Petersen, W. and B. Tillmann, Collagenous fibril texture of the human knee joint menisci. Anat Embryol (Berl), 1998. 197(4): p. 317-24.
6. Baratz, M.E., F.H. Fu, and R. Mengato, Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med, 1986. 14(4): p. 270-5.
7. Lanzer, W.L. and G. Komenda, Changes in articular cartilage after meniscectomy. Clin Orthop Relat Res, 1990(252): p. 41-8.
8. Fairbank, T.J., Knee joint changes after meniscectomy. J Bone Joint Surg Br, 1948. 30b(4): p. 664-70.
9. Metcalf, R.W., Arthroscopic meniscal surgery., in Operative Arthroscopy., M. JB, Editor. 1991, Raven Press: New York. p. pp. 203–236.
10. Salata, M.J., A.E. Gibbs, and J.K. Sekiya, A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med, 2010. 38(9): p. 1907-16.
11. Hede, A., E. Larsen, and H. Sandberg, Partial versus total meniscectomy. A prospective, randomised study with long-term follow-up. J Bone Joint Surg Br, 1992. 74(1): p. 118-21.
12. Tapper, E.M. and N.W. Hoover, Late results after meniscectomy. J Bone Joint Surg Am, 1969. 51(3): p. 517-26 passim.
13. Ihn, J.C., S.J. Kim, and I.H. Park, In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop, 1993. 17(4): p. 214-8.
14. Vadher, S.P., et al., Finite element modeling following partial meniscectomy: effect of various size of resection. Conf Proc IEEE Eng Med Biol Soc, 2006. 1: p. 2098-101.
15. Jones, R.S., et al., Direct measurement of hoop strains in the intact and torn human medial meniscus. Clin Biomech (Bristol, Avon), 1996. 11(5): p. 295-300.
16. Petty, C.A. and J.H. Lubowitz, Does arthroscopic partial meniscectomy always cause arthritis? Sports Med Arthrosc, 2012. 20(2): p. 58-61.
17. Burks, R.T., M.H. Metcalf, and R.W. Metcalf, Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy, 1997. 13(6): p. 673-9.
18. McDermott, I.D. and A.A. Amis, The consequences of meniscectomy. J Bone Joint Surg Br, 2006. 88(12): p. 1549-56.
19. Rockborn, P. and J. Gillquist, Long-term results after arthroscopic meniscectomy. The role of preexisting cartilage fibrillation in a 13 year follow-up of 60 patients. Int J Sports Med, 1996. 17(8): p. 608-13.
20. Chatain, F., et al., The natural history of the knee following arthroscopic medial meniscectomy. Knee Surgery, Sports Traumatology, Arthroscopy, 2000. 9(1): p. 15-18.
21. Englund, M. and L.S. Lohmander, Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum, 2004. 50(9): p. 2811-9.
22. Small, N.C., Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy, 1988. 4(3): p. 215-21.
23. Allum, R., Complications of arthroscopy of the knee. J Bone Joint Surg Br, 2002. 84(7): p. 937-45.
24. Papalia, R., et al., Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull, 2011. 99: p. 89-106.
| How to Cite this article: Patil SS, Tapasvi SR, Shekhar A. Meniscectomy-Outcomes and Complications. Asian Journal of Arthroscopy Aug – Nov 2016 |