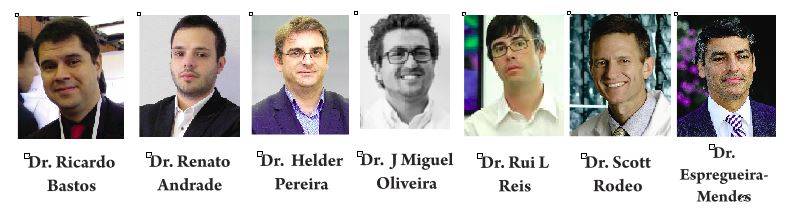
Ricardo Bastos, Renato Andrade, Hélder Pereira, J Miguel Oliveira, Rui L Reis, Scott Rodeo, João Espregueira-Mendes.
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 47-52.
Author: Ricardo Bastos[1,2,3], Renato Andrade[2,3,4], Hélder Pereira[5,6,7,8], J Miguel Oliveira, Rui L Reis, Scott Rodeo, João Espregueira-Mendes[2,3,5,6,14].
[1] Universidade Federal Fluminense, Nireói, Rio de Janeiro, Brazil.
[2] Clínica do Dragão, Espregueira-Mendes Sports Centre – FIFA Medical Centre of Excellence, Porto, Portugal.
[3] Dom Henrique Research Centre, Porto, Portugal.
[4] Faculty of Sports, University of Porto, Porto, Portugal.
[5] 3B’s Research Group – Biomaterials, Biodegradables and Biomimetics, University of Minho, Headquarters of the European Institute of Excellence on Tissue Engineering and Regenerative Medicine, AvePark- Parque de Ciência e Tecnologia, 4805-017 Barco, Guimarães, Portugal.
[6] – ICVS/3B’s – PT Government Associated Laboratory, Braga/Guimarães, Portugal.
[7] – Orthopaedic Department, Centro Hospitalar Póvoa de Varzim – Vila do Conde, Póvoa de Varzim, Portugal.
[8] – Ripoll y De Prado Sports Clinic FIFA Medical Centre of Excellence, Murcia-Madrid, Spain.
[9] – Co-Chief Emeritus, Sports Medicine and Shoulder Service, Hospital for Special Surgery, New York, USA.
[10] – Co-Director, Tissue Engineering, Regeneration, and Repair Program, New York, USA.
[11] – Orthopaedic Surgery, Weill Medical College of Cornell University, New York, USA.
[12] – Attending Orthopaedic Surgeon, Hospital for Special Surgery, New York, USA.
[13] – Head Team Physician, New York Giants Football, New York, USA.
[14] – Orthopaedics Department of Minho University, Minho, Portugal.
Address of Correspondence
Dr. João Espregueira-Mendes; Via Futebol Clube do Porto – F. C. Porto Stadium, Porto, Portugal; +351 220 100 100; Email: espregueira@dhresearchcentre.com
Abstract
Despite the high incidence, meniscal lesions still remain a clinical challenge due to its limited regenerative ability. In the last two decades, the development of scaffolding strategies has revolutionized meniscus treatment possibilities. Along with these new developments, the orthopaedic community has embraced the campaign “preserve the meniscus”. In this sense, acellular or cellularized scaffolds have emerged as a potential solution to treat irreparable meniscal lesions. Herein, it are overviewed the up-to-date acellular meniscal scaffolds used in the clinics, indications and discussed their outcomes.
Keywords: Meniscal scaffolds; Meniscal implants; Meniscal substitutes.
Introduction
The menisci have been described as a two-edge shaped semilunar discs of fibrocartilaginous tissue, found at the medial and lateral compartment of the tibiofemoral joint (1, 2). They play a fundamental role in many aspects of knee function, including articular congruency and stability, load distribution, shock absorption as well as a role in joint lubrication and proprioception (3). Many of these functions are achieved through the ability to transmit and distribute load over t The medial anhe tibial plateaus.d lateral menisci can transmit from 50% up to 70% of the load when the knee is in extension, and up to 85% at 90 degrees of knee flexion (4). Removal of the medial meniscus can result in a 50% to 70% reduction in femoral condyle cartilage contact area and a 100% increase in contact stress (5). Total lateral meniscectomy causes a 40% to 50% decrease in cartilage contact area and increases contact stress in the lateral compartment up to 200% to 300% of normal. Furthermore, even just partial removal of the meniscus does alter joint loading, particularly when two thirds of the posterior horn is excised (6). Despite the importance of the meniscus structure and the need for its preservation, meniscal lesions are the most common surgically treated knee pathology, and their annual incidence can be estimated at 60-70 per 100,000 knees, with 850,000 meniscal procedures performed yearly only in the United States (7) and 400,000 in Europe (8). For several years, the meniscus function was not fully understood. Recent pre-clinical and clinical evidences support the idea that the preservation of the meniscus structure is of outmost importance (9, 10). Thus, tissue engineering approaches have gain great attention as promise to regenerate different tissues and organs, including meniscus tissue (11-15). It has provided a fundamental understanding and technology that have permitted the development of scaffolds derived from biological tissues and synthetic materials, and there is currently a large amount of active, ongoing research into meniscus scaffolds (16-18). The meniscus scaffolds have been mainly limited to the treatment of meniscus partial repair once it requires an undamaged meniscal rim and enough tissue at the anterior and posterior horns to allow the fixation of the scaffold to the remaining meniscal tissues.
Types of Scaffolds
Scaffold biomechanical structure must have adequate material properties to allow tissue regeneration, while protecting the newly-forming tissue from excessive stresses. Their absorption must be sufficiently gradual, allowing appropriate cell migration, formation of new vessels, and matrix synthesis in order to create meniscal-like tissue (19, 20). At the same time, the scaffold and its degradation products should not damage the articular surface or invoke a foreign body reaction. An important step in the preparation of acellular meniscal scaffolds is the ability of mimicking the architectural and geometric complexity of the native tissue (20, 21). In this sense, it is crucial to further understand the menisci anatomy, biology, ultrastructure and biomechanical function to enhance the success of the meniscal substitution (1, 13). Two scaffolds are currently in clinical use.
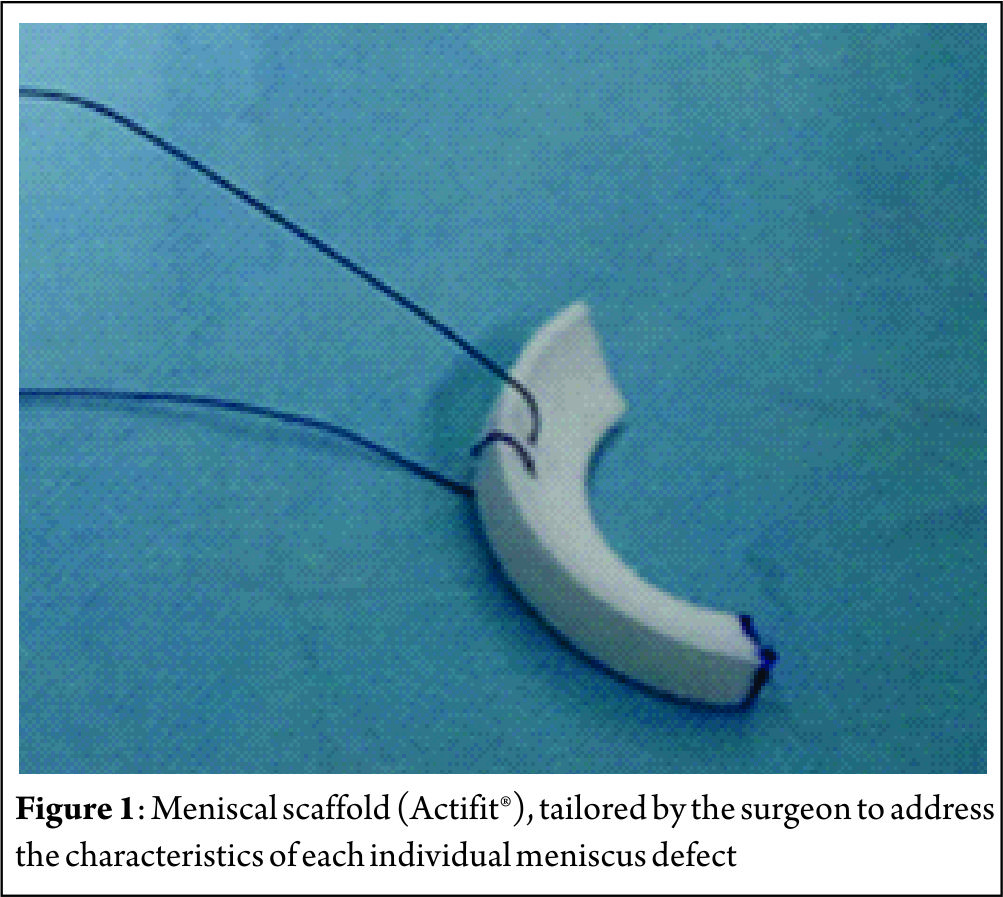
Collagen Meniscus Implant (CMI, Ivy Sports Medicine GmbH, Germany) – First published in 1997, CMI is a type-I collagen (isolated and purified from bovine Achilles tendon) scaffold (22) to which glycosaminoglycans are added. It has a meniscus-like shape, is implantable arthroscopically, and it is biocompatible and biodegradable. It has a microscopic porous structure that allows cellular ingrowth, induces differentiation and proliferation of fibrocartilaginous cells, leading to the creation of a meniscus-like tissue, concomitant with gradual resorption of the scaffold. Nevertheless, collagen scaffolds are fragile during the implant procedure, and have shown a decrease in size on follow-up magnetic resonance image (MRI) and arthroscopic second look follow-up. The second type of scaffold is Actifit® (Orteq, United Kingdom) that has been developed to overcome the perceived limitations of CMI related to difficulties in tissue handling with respect to suturing during implantation (Figure 1). Actifit® is composed of a slowly degrading polymer with polycaprolactone and urethane segments (23). Its structure seems to have better mechanical properties and is more resistant to sutures and loads as compared to CMI. The scaffold is 80% porous; the remaining 20% are made of a polymer with a low absorption rate. Degradation starts with hydrolysis of polycaprolactone segments, which lasts up to five years; the polyurethane segments are removed by macrophages and giants cells or integrated into surrounding tissues (24, 25).
Indications – Contraindications
When considering meniscal scaffolding, the surgeon should take into account several individual aspects, such as the patient’s age and weight, status of meniscal degeneration or concomitant conditions (such as axial malalignment and ligamentous insufficiency) (26). In this sense, several indications and contraindications have been developed as summarized in Table 1.

Preoperative Preparation
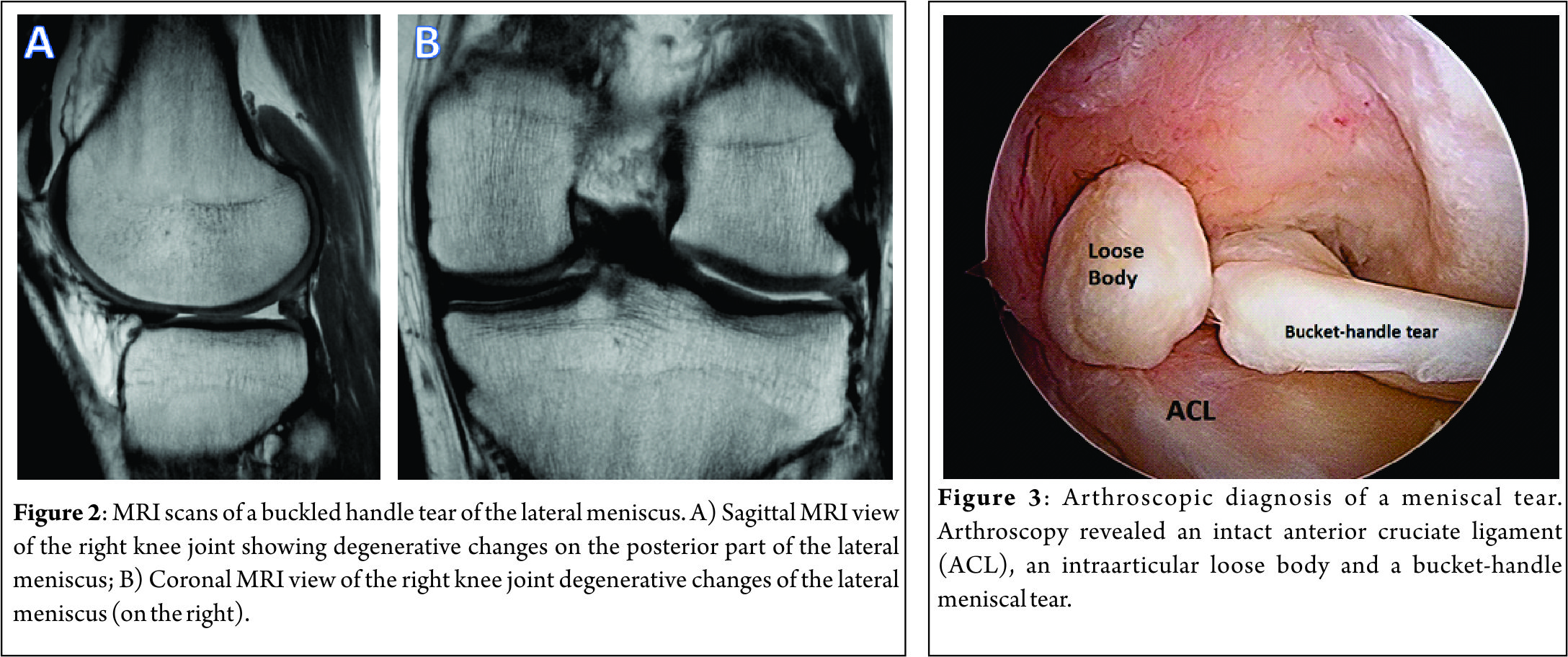
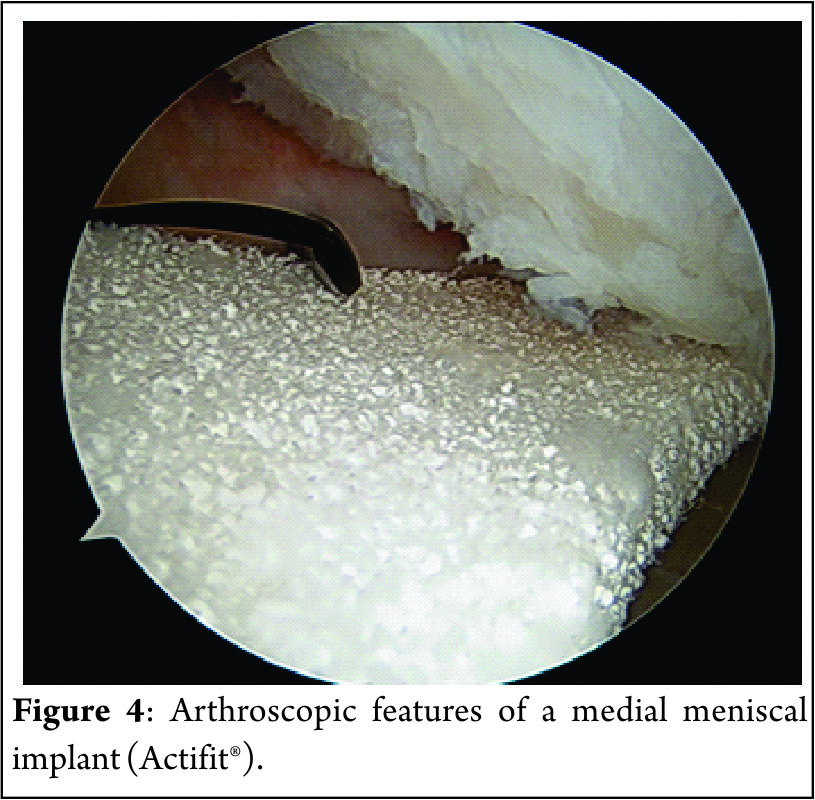
The preoperative imaging preparation usually involves radiography, MRI and, in some special cases, an arthro-computed tomography (arthro-CT). The radiographic imaging studies usually include bilateral comparison of weight-bearing radiographs (antero-posterior, lateral, Schuss or Rosenberg views). The MRI is usually performed to assess the cartilaginous structures status, quantify the meniscal damage, as well as the presence of bone marrow edema and/or meniscal extrusion (Figure 2). The arthro-CT scan may complement the MRI studies by assessing the meniscal volume and chondral damage (26). The imaging studies should be complemented with a comprehensive clinical examination of the knee. Special attention should be given to the knee ligament stability, as this has several implications in the meniscal surgery. In addition, diagnostic arthroscopy (Figure 3) may be performed to further assess the meniscal status and decide upon the best technique (26).
Surgical Technique
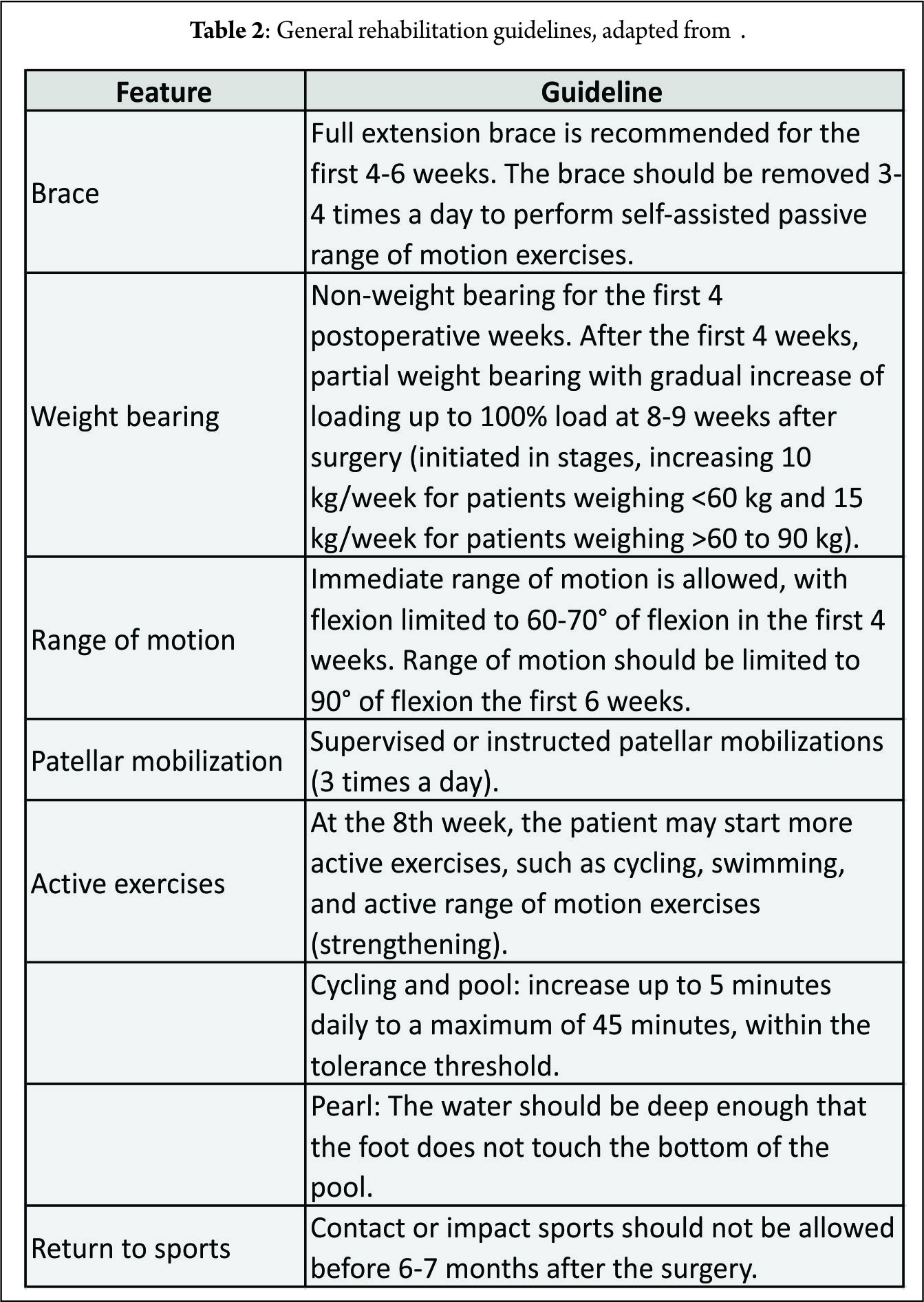
The procedure can be performed arthroscopically using the two standard anteromedial and anterolateral portals. The portals should be enlarged for an easier passage of the scaffold. The native remaining meniscus is thoroughly evaluated, and any torn or degenerative tissue is removed in order to leave a healthy and uniform meniscal rim, ensuring that the resulting defect site extends into the vascularized red-on-red or red-on-white zone of the meniscus. The meniscal rim is punctured in order to create vascular access channels. Gentle rasping of the synovial lining may further stimulate meniscal integration and tissue ingrowth. The exact size of the defect is measure with a flexible rod loaded in a rigid cannula starting at the posterior end of the lesion. The scaffold is measured and trimmed to the correct size on the sterile field of the operating environment (10% larger than in situ measurement to compensate for the shrinkage caused by suturing of the sponge-like material and to assure a snug optimal fit into the prepared defect). In order to achieve a perfect fit of the scaffold with the native meniscus at the anterior junction, the anterior side should be cut at an oblique angle of 30°-45°. The implant is inserted into the defect (Figure 4). Standard arthroscopic meniscal suturing techniques may be utilized for scaffold stabilization. The authors prefer “all-inside” vertical stitches placed every 4 to 5 mm to suture the scaffold along the periphery. The anterior and posterior scaffold extremities are fixed to the native remnant with horizontal stitches.
Concomitant Surgeries
Since other associated deficiencies (such as axial malalignment or ligamentous instability) may lead to poorer outcomes following meniscal surgery, these should be address in combination with the meniscal substitution (27). Anterior cruciate ligament insufficiency, if not addressed, may result in residual laxity, which may lead to an unfavorable meniscal healing environment. In this sense, ACL reconstruction has been performed along with the meniscal substitution in up to 67% of the patients (28-30). When performing concomitant ACL reconstruction, the meniscal bed should be firstly prepared and then the tibial and femoral tunnels may be drilled. After the tunnels are drilled, the ACL graft is passed through the tunnels and fixed at the femoral site, as the meniscal scaffold is inserted and sutured. Subsequently, the ACL graft is fixed at the tibial site with 20° of knee flexion (31). When uncorrected axial knee malalignments are found, these should be concomitantly or previously corrected. In a varus malalignment situation, a high tibial osteotomy may be performed to correct the malalignment. Special attention must be directed to the tibial slope and proper release of the medial collateral ligament should be performed. In valgus malalignments, if the deformity does not involve the tibial bone, osteotomy is done on the femoral side to avoid joint line obliquity (27).
Rehabilitation protocol
Patients are required to undergo a conservative rehabilitation program similar to that for a meniscal allograft. Special attention is required when the meniscal scaffold is implanted with concomitant ACL reconstruction or realignment osteotomy. In these cases, a rehabilitation program should be tailored to comply with the concomitant procedures postoperative particularities (26, 27). General guidelines for the rehabilitation program are presented in Table 3.
Clinical Studies
Although the literature contains clinical studies (33-35) that support the use of meniscal scaffold implantation for the treatment of irreparable meniscal tears, the quality of the studies is generally low, with lack of randomized trials and long-term follow-up to confirm clinical benefit and the most appropriate indications. Furthermore, long-term follow-up studies are required to verify the protective effect on the damaged joint compartment exerted by meniscal scaffold implantation.
A recent systematic literature review (35) analyzed results and indications for the treatment of meniscal loss. There has been an increase in publications regarding this topic recently, and the authors concluded that both CMI and Actifit seem to be safe and positive results have been shown for both scaffolds. Bulgheroni et al. (36) evaluated the safety and effectiveness of the polyurethane meniscal scaffold through clinical examination, MRI and arthroscopic second look, over a minimum two-year follow-up and showed no adverse reactions to the implant. The implant showed clear, hyperintense signal, sometimes irregular, and the chondral surface was preserved in all cases. At arthroscopic second look at 12 and 24 months, the scaffold was found to have an irregular morphology and to be slightly reduced in size. Zafagnini et al. (37), in a 10-year follow-up study, compared the medial collagen meniscus implant versus partial medial meniscectomy. The CMI group showed significantly lower visual analog scale scores for pain and higher objective International Knee Documentation Committee and Tegner index scores. Radiographic evaluation showed significantly less medial joint space narrowing in the CMI group compared to partial medial meniscectomy. No significant differences between groups were reported regarding Lysholm and Yulish scores. Another long-term study compared outcomes of CMI versus partial meniscectomy in patients with concomitant ACL reconstruction. The authors concluded that patients with chronic meniscal tears treated with medial CMI reported lower levels of post-operative pain compared to meniscectomy, while acute lesions treated with CMI showed less knee laxity at follow-up (38). The CMI when performed in the acute setting showed no additional benefits when compared to partial medial meniscectomy alone (28).
Zafagnini et al. (39), in a multi-center study, evaluated the clinical outcomes of 43 patients after lateral CMI implantation. They reported improvement of all clinical scores from baseline to follow-up evaluations. At the final follow-up, 58% of the patients reported activity levels comparable to their pre-injury values, with 95% patient reported satisfaction. A higher body mass index, the presence of concomitant procedures, and a chronic injury pattern were identified as potential negative prognostic factors.
As far as concomitant open-wedge high tibial osteotomies is concerned, Gelber et al. (40) found no short-term additional benefit when compared to partial meniscectomy and meniscal scaffolding.
Final Remarks and Future Directions
The menisci are known to be heterogeneous complex structures with segmental variations according to their anatomy, biology and function. The proper understanding on the different types of meniscal injuries (both traumatic and degenerative) and their pathophysiology and pathomechanics will assist the clinician in identifying the correct indications and contraindication for each type of lesion, preserving the meniscus whenever possible. The clinical application of meniscal scaffolds is limited to CMI and Actifit. In order to successfully implant these meniscus scaffolds, it is required an intact meniscal rim and sufficient meniscal tissue at the anterior and posterior meniscus horns to attach the scaffold. When in case of axial malalignments and/or ligament insufficiencies, these must be correct prior or during the scaffold implantation. The rehabilitation protocol should be tailored to address each patient’s individual characteristics, respect the chronobiology of the scaffold tissue integration and the progression within phases should be goal-based. Novel meniscal scaffolds have been developed for addressing total meniscus reconstruction with a functional meniscus replacement, mimicking the biology and mechanical properties of the native meniscus. These novel scaffolds may further protect the articular cartilage surface of the knee joint from the extensive damage after a total meniscectomy. A second generation of implants pre-cultured in vitro allows cell adhesion and extracellular matrix production and then are implanted into the meniscal defects which will probably follow as cell seeding as has been demonstrated to improve the mechanical properties and histological results. In the future, it may be possible to improve tissue formation in the meniscal scaffold using autologous cells (e.g., stem cells) and/or growth factors (e.g., platelet-rich plasma). This strategy may augment the tissue regeneration and improve clinical results. The use of mesenchymal stem cells may also enhance a greater promotion of intrinsic meniscal healing capacity. In addition, nanotechnology and gene therapy have emerged as potential options and have showed great potential for the treatment of meniscal lesions, however its translation into the clinical setting may take a few more years. Biofabrication of patient-specific meniscal scaffolds with a 3D printer from the advanced segmentation of menisci knee MRI datasets has been showing promising results in the laboratory setting. This novel technique will allow tailoring the meniscal scaffold to the patient-specific native characteristics of the knee.
References
1. Pereira H, Cengiz IF, Silva-Correia J, Cucciarini M, Gelber PE, Espregueira-Mendes J, Oliveira JM, Reis, RL. Histology-Ultrastructure-Biology. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 23-33.
2. Halewood C, Amis AA. Physiology: Biomechanics. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 35-45.
3. Heijink A, Gomoll AH, Madry H, Drobnič M, Filardo G, Espregueira-Mendes J, van Dijk CN. Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):423-35.
4. Ahmed A, Burke D. In-vitro of measurement of static pressure distribution in synovial joints—Part I: Tibial surface of the knee. J Biomech Eng. 1983;105(3):216-25.
5. Watanabe Y, Van Scyoc A, Tsuda E, Debski RE, Woo SL. Biomechanical function of the posterior horn of the medial meniscus: a human cadaveric study. J Orthop Sci. 2004;9(3):280-4.
6. Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomech Eng. 1983;5(2):157-61.
7. Abrams GD, Frank RM, Gupta AK, Harris JD, McCormick FM, Cole BJ. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med. 2013:0363546513495641.
8. Verdonk PC, Dhollander AA, Tampere T, Verdonk R. Meniscus Substitution: Scaffolds, Allografts and Prosthetic Implants. In: Emans PJ, Peterson L, editors. Developing Insights in Cartilage Repair. Springer; 2014. p. 253-65.
9. Verdonk R. The meniscus: past, present and future. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):145-6.
10. Di Matteo B, Tarabella V, Filardo G, Viganò A, Tomba P, Marcacci M. Thomas Annandale: the first meniscus repair. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1963-6.
11. Pereira H, Frias AM, Oliveira JM, Espregueira-Mendes J, Reis RL. Tissue engineering and regenerative medicine strategies in meniscus lesions. Arthroscopy. 2011;27(12):1706-19.
12. Cengiz IF, Pereira H, Pêgo JM, Sousa N, Espregueira‐Mendes J, Oliveira JM, Reis RL. Segmental and regional quantification of 3D cellular density of human meniscus from osteoarthritic knee. J Tissue Eng Regen Med. 2015. doi: 10.1002/term.2082.
13. Pereira H, Caridade S, Frias A, Silva-Correia J, Pereira D, Cengiz I, Mano JF, Oliveira JM, Espregueira-Mendes, J, Reis, RL. Biomechanical and cellular segmental characterization of human meniscus: building the basis for Tissue Engineering therapies. Osteoarthritis Cartilage. 2014;22(9):1271-81.
14. Cengiz IF, Pitikakis M, Cesario L, Parascandolo P, Vosilla L, Viano G, Oliveira, JM, Reis, RL. Building the Basis for Patient-Specific Meniscal Scaffolds: From Human Knee MRI to Fabrication of 3D Printed Scaffolds. Bioprinting. 2016.
15. Pereira H, Cengiz IF, Silva-Correia J, Oliveira JM, Reis RL, Espregueira-Mendes J. Human meniscus: from biology to tissue engineering strategies. In: Doral MN, Karlsson J, editos. Sports Injuries. Springer; 2015. p. 1089-102.
16. Yan L-P, Oliveira JM, Oliveira AL, Caridade SG, Mano JF, Reis RL. Macro/microporous silk fibroin scaffolds with potential for articular cartilage and meniscus tissue engineering applications. Acta Biomater. 2012;8(1):289-301.
17. Yan L-P, Silva-Correia J, Oliveira MB, Vilela C, Pereira H, Sousa RA, Mano JF, Oliveira AL, Oliveira JM, Reis, RL. Bilayered silk/silk-nanoCaP scaffolds for osteochondral tissue engineering: in vitro and in vivo assessment of biological performance. Acta Biomater. 2015;12:227-41.
18. Bacelar AH, Cengiz IF, Silva-Correia J, Sousa RA, Oliveira JM, L. RR. “Smart” Hydrogels in Tissue Engineering and Regenerative Medicine Applications. In: Khang G, editor. Handbook of Intelligent Scaffolds for Regenerative Medicine. Pan Stanford Publishing; 2015.
19. Buma P, Ramrattan N, van Tienen TG, Veth RP. Tissue engineering of the meniscus. Biomaterials. 2004;25(9):1523-32.
20. Reguzzoni M, Manelli A, Ronga M, Raspanti M, Grassi FA. Histology and ultrastructure of a tissue‐engineered collagen meniscus before and after implantation. J Biomed Mater Res B Appl Biomater. 2005;74(2):808-16.
21. Pereira H, Silva-Correia J, Oliveira J, Reis R, Espregueira-Mendes J. Future trends in the treatment of meniscus lesions: from repair to regeneration. In: Verdonk R, Espregueira-Mendes J, Monllau, JC, editors. Meniscal Transplantation. Springer; 2013. p. 103-12.
22. Stone KR, Steadman JR, Rodkey WG, Li S-T. Regeneration of Meniscal Cartilage with Use of a Collagen Scaffold. Analysis of Preliminary Data. J Bone Joint Surg Am. 1997;79(12):1770-7.
23. Verdonk R, Verdonk P, Huysse W, Forsyth R, Heinrichs E-L. Tissue ingrowth after implantation of a novel, biodegradable polyurethane scaffold for treatment of partial meniscal lesions. Am J Sports Med. 2011;39(4):774-82.
24. Van Minnen B, Van Leeuwen M, Kors G, Zuidema J, Van Kooten T, Bos R. In vivo resorption of a biodegradable polyurethane foam, based on 1, 4‐butanediisocyanate: A three‐year subcutaneous implantation study. J Biomed Mater Res A. 2008;85(4):972-82.
25. Zuidema J, van Minnen B, Span M, Hissink C, van Kooten T, Bos R. In vitro degradation of a biodegradable polyurethane foam, based on 1, 4‐butanediisocyanate: A three‐year study at physiological and elevated temperature. J Biomed Mater Res A. 2009;90(3):920-30.
26. Pujol N, Verdonk P. Actifit Polyurethane Meniscus Scaffold: Basic Science, Techniques, and Results. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 543-51.
27. Hinarejos P, Erggelet C, Monllau JC. Collagen Meniscus Implant: Basic Science, Technique and Results. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 531-42.
28. Rodkey WG, DeHaven KE, Montgomery WH, Baker CL, Beck CL, Hormel SE, Steadman R, Cole B, Briggs K. Comparison of the collagen meniscus implant with partial meniscectomy. J Bone Joint Surg Am. 2008;90(7):1413-26.
29. Monllau JC, Gelber PE, Abat F, Pelfort X, Abad R, Hinarejos P, et al. Outcome after partial medial meniscus substitution with the collagen meniscal implant at a minimum of 10 years’ follow-up. Arthroscopy. 2011;27(7):933-43.
30. Hirschmann M, Keller L, Hirschmann A, Schenk L, Berbig R, Lüthi U, et al. One-year clinical and MR imaging outcome after partial meniscal replacement in stabilized knees using a collagen meniscus implant. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):740-7.
31. Monllau JC. Collagen Meniscal Implant (CMI). In: Verdonk R, Espregueira-Mendes J, Monllau, JC, editors. Meniscal Transplantation. Springer; 2013. p. 73-82.
32. Implant MCM. Rehabilitation program summary for patients, surgeons, and physiotherapists. Franklin Lakes, NJ, USA: ReGen Biologics, Inc.; 2006.
33. Grassi A, Zaffagnini S, Muccioli GMM, Benzi A, Marcacci M. Clinical outcomes and complications of a collagen meniscus implant: a systematic review. Int Orthop. 2014;38(9):1945-53.
34. Zaffagnini S, Grassi A, Muccioli GMM, Bonanzinga T, Nitri M, Raggi F, Ravazzolo J, Marcacci, M. MRI evaluation of a collagen meniscus implant: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3228-37.
35. Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M. Meniscal scaffolds: results and indications. A systematic literature review. Int Orthop. 2015;39(1):35-46.
36. Bulgheroni P, Bulgheroni E, Regazzola G, Mazzola C. Polyurethane scaffold for the treatment of partial meniscal tears. Clinical results with a minimum two-year follow-up. Joints. 2013;1(4):161.
37. Zaffagnini S, Muccioli GMM, Lopomo N, Bruni D, Giordano G, Ravazzolo G, et al. Prospective Long-Term Outcomes of the Medial Collagen Meniscus Implant Versus Partial Medial Meniscectomy A Minimum 10-Year Follow-Up Study. Am J Sports Med. 2011;39(5):977-85.
38. Bulgheroni E, Grassi A, Bulgheroni P, Muccioli GMM, Zaffagnini S, Marcacci M. Long-term outcomes of medial CMI implant versus partial medial meniscectomy in patients with concomitant ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3221-7.
39. Zaffagnini S, Grassi A, Muccioli GMM, Holsten D, Bulgheroni P, Monllau JC, Berbig R, Lagae K, Crespo R, Marccaci M. Two-year clinical results of lateral collagen meniscus implant: a multicenter study. Arthroscopy. 2015;31(7):1269-78.
40. Gelber PE, Isart A, Erquicia JI, Pelfort X, Tey-Pons M, Monllau JC. Partial meniscus substitution with a polyurethane scaffold does not improve outcome after an open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):334-9..
| How to Cite this article: Bastos R, Andrade R, Pereira H, Oliveira JM, Reis RL, Rodeo S, Espregueira-Mendes J. Meniscal Scaffolds in the Clinics: Present and future trends.Asian Journal of Arthroscopy Aug – Nov 2016;1(2):47-52 . |


Meniscus Ramp Lesion
Bertrand Sonnery Cottet, Sanesh Tuteja, Nuno Camelo Barbosa, Mathieu Thaunat
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 28-34.
Author: Bertrand Sonnery Cottet[1], Sanesh Tuteja[1], Nuno Camelo Barbosa[1], Mathieu Thaunat[1].
[1] Investigation performed at the Centre Orthopédique Santy, FIFA medical center of Excellence, Groupe Ramsay-Générale de Santé, Lyon, France
Address of Correspondence
Dr Bertrand Sonnery-Cottet
Centre Orthopédique Santy, 24 Avenue Paul Santy, Lyon, 69008, France
Email: sonnerycottet@aol.com.
Abstract
Ramp Lesions of the Medial Meniscus (MM) are associated with 9 to 17% of ACL Tears and are seldom recognized on preoperative magnetic resonance imaging (MRI) scans. They also often remain undiagnosed when viewing from the standard anterior compartment arthroscopic portals. Improved visualization is the key to achieving good meniscal repair results as it improves diagnosis of longitudinal tears in posterior horn MM, safeguards better debridement prior to repair and ensures good approximation of the torn ends under vision. A systematic posteromedial exploration allows discovery of and debridement of the hidden MM lesion and repair with a suture hook device is associated with low morbidity and must be undertaken whenever possible.
Keywords: Medial meniscus, Ramp lesion, Repair, Healing, Anterior cruciate ligament, Knee.
Introduction
Meniscal lesions of the posterior horn of medial meniscus (MM) are very often associated with an ACL rupture (16,32,49). Certain specific lesions of the Medial Meniscus (MM) such as meniscosynovial or meniscocapsular tears and meniscotibial ligament lesions are associated with 9 to 17% of ACL Tears (8,21) and are seldom recognized on preoperative magnetic resonance imaging (MRI) scans (8,38). They also often remain undiagnosed when viewing from the standard anterior compartment arthroscopic portals including a probing. They were named in the 1980s by Strobel et al (42) as ‘‘Ramp’’ lesions of the meniscus and have drawn a lot of attention over the past few years (3,8,21,38,42). The aim of this article will be to write a narrative review of this Ramp meniscal lesion.
History
Hamberg et al (15) first described “a peripheral vertical rupture in the posterior horn of the medial or lateral meniscus with an intact body” in 1983. They repaired these lesions through a postero-medial vertical arthrotomy; with the belief that the capillary blood supply from the capsule aids healing of the meniscus. They reported promising results (84% healing) in old and new lesions alike, thus providing some valuable insight into the philosophy of meniscal conservation. Morgan et al (25) in 1991 described the first arthroscopic vertical suture of the PHMM using Polydioxanone (PDS) sutures with an outside-to-inside technique. They reported a 16% failure rate occurring in patients with a concurrent ACL injury. They proposed that the rotation axis of the knee joint was altered in an ACL deficit knee thus placing excessive loads on the posterior horn of the medial meniscus. The kinematics of the posterior horn of the medial meniscus in the ACL deficient knee was therefore not conducive to meniscal healing after repair despite a peripheral blood supply. They also noted that, when combined with an ACL reconstruction, peripheral meniscal repair healing rates improved and approached those obtained in an ACL intact knee (25). Ahn et al (5) in 2004 described the first clinical series of an arthroscopic all-inside suture technique for tears in posterior horn of medial meniscus. Using a suture hook thorough 2-posteromedial portals, PHMM tears were repaired with concurrent reconstruction of the ACL. They concluded that the arthroscopic all-inside vertical suture using a hook resulted in a high healing rate even in large and complex vertical tears. Seil et al (38) in 2009 highlighted the indications for meniscal repairs based on the presence of associated ligamentous injuries and morphology of the lesion.
They advocated that Meniscal repairs be ‘‘ideally’’ carried out in:
1. Young patients (< 40 years)
2. No associated joint degeneration.
3. Vertical lesions in the peripheral third of the meniscus (3mm of the meniscosynovial junction) (4) and in conjunction with an ACL reconstruction.
4. Significantly displaced bucket-handle tear or an MMPH tear with vertical step off (5).
Epidemiology
The prevalence for a meniscal lesion with an ACl tear has been reported between 47% to 61% (13,14). In 2010, S. Bollen et al (8) reported menisco-capsular lesions in 9.3% of their prospective series of 183 ACL reconstructions whereas Liu et al (21) described a prevalence of 16.6% in a series of 868 consecutive ACL reconstructions. In our series (40) on ACL deficient knees, a meniscal tears was identified in 125 out of the 302 patients. Following a systematic algorithm for exploration of the knee joint (Figure. 1), we found that; 75 (60%) medial meniscal body lesions were diagnosed through a standard anterior portal exploration, 29 (23.2%) ramp lesions were diagnosed during exploration of the posteromedial compartment, and 21 (16.8%) were discovered by probing the tear through a posteromedial portal and after minimal debridement of a superficial soft tissue layer with a motorized shaver. All-in-all, 42% (21/50) of the lesions diagnosed via inspecting the posterior compartment appeared only after superficial soft tissue debridement and were classified as ‘‘hidden lesions.’’ An ACL injury with an age at presentation above 30 years, male sex and a delay between injury and surgery are considered risk factors for concomitant meniscal lesions (8).
Biomechanical Implication on ACL
The importance of the meniscus in stabilizing the knee joint in chronically ACL-deficient knees has been validated by multiple studies (9, 39). A Peripheral posterior horn tear is caused by the recurrent trauma sustained by the Medial Meniscus, which acts as a ‘‘bumper’’ in ACL-deficient knees (2). In addition, contraction of the semimembranosus at its insertion along the posteromedial capsule may stress the peripheral meniscus, resulting in meniscocapsular tearing (17). This could occur at the time of injury or during subsequent instability episodes in the subacute or chronic situation (43). A capsular injury might also occur during the so-called medial contrecoup injury (18) after subluxation of the lateral tibial plateau and during subsequent reduction of the tibia (41). A longitudinal tear of the PHMM in ACL-deficient knees increases the anterior translation of the tibia and a repair of this lesion reduces Anteroposterior tibial translation significantly at most flexion angles (17) and most prominently at 30 degrees of flexion (12, 30). Peltier et al (30) observed that the PHMM was stabilised by the meniscotibial ligament posteriorly, which in turn inserted onto the posterior aspect of the proximal tibia. The capsule of the knee joint inserts more distally on this posterior surface. The posterior capsule hence lacks insertion onto the posterior aspect of the PHMM. Detachment of the ligament therefore results in an abnormal mobility of the entire PHMM, producing rotational instability. The authors observed that the division of the menisco-tibial ligament resulted in a statistically significant increase in internal tibial rotation. Such lesions occur either in the mid-substance (repairable) or as a bony avulsion (irreparable). Stephen et al (41) reported that the anterior tibial translation and external rotation were both significantly increased compared with the ACL-deficient knee after posterior meniscocapsular sectioning and these parameters were not restored after ACL reconstruction alone but were restored with ACL reconstruction combined with posterior meniscocapsular repair.
Classification [46] (Figure. 2)
We have proposed a classification for ramp lesions which is as follows:
Type 1: Ramp lesions. Very peripherally located in the synovial sheath. Mobility at probing is very low. (B)
Type 2: Partial superior lesions. It is stable and can be diagnosed only by trans-notch approach. Mobility at probing is low. ©
Type 3: Partial inferior or hidden lesions. It is not visible with the trans-notch approach, but it may be suspected in case of mobility at probing, which is high. (D)
Type 4: Complete tear in the red-red zone. Mobility at probing is very high. (E)
Type 5: Double tear.
Surgical Technique (46)
With the patient supine on the operating table, a tourniquet is placed high on the thigh, and the knee placed at 90º of flexion with a foot support to allow full range of knee motion. Using standard arthroscopy portals, high lateral as viewing and medial portal for instrumentation, articular inspection is performed and we engage a probe in the posterior segment of the meniscus and force an anterior excursion of the meniscus. If the meniscus subluxates under the condyle, it is an indicator for instability and an indirect sign of a ramp lesion. Direct visualization of the posteromedial compartment is mandated to diagnose and repair these lesions. Even if the meniscus appears stable on probing, a systematic exploration of the posterior segment must be performed using the protocol in (Figure.1) Through a Guillquist maneuver, the arthroscope in the anterolateral portal is advanced in the triangle formed by the medial femoral condyle, the posterior cruciate ligament, and the tibial spines. With valgus force applied initially in flexion followed by knee extension, the arthroscope is pass through the space at the condyle border of the medial femoral condyle. Internal rotation applied to the tibia further enhances visualization; this causes subluxation of the posterior tibial plateau causing a posterior translation of the middle third segment. Almost two-thirds of peripheral lesions can be diagnosed with this maneuver. Tears of the posterior segment must be approached posteromedially. The posteromedial portal is placed superior to the hamstring tendons and posterior to the medial joint line, also trans illumination allows observation of the great saphenous vein, that is in close relation to the infra-patellar branch of the internal saphenous nerve, that must be avoided. The needle is introduced from outside to inside, in the direction of the lesion. The portal is prepared with a number 11blade scalpel under arthroscopic control. The all-inside suture is accomplished with or without a working cannula, depending on the surgeons choice. Using a shaver the lesion is debrided and the intervening fibrous tissue is excised. Suturing is carried out using a 25º curved hook (Suture Lasso, Arthrex): a left curved hook is used for a right knee and vice versa. The curved hook is loaded with a no. 2 non-absorbable braided composite suture (Fiberwire, Arthrex) or a absorbable no.1 PDS introduced through the posteromedial portal. The curved hook must penetrate the peripheral wall of the MM, and then the inner wall of the MM. The free end of the suture in the posteromedial space is grasped and brought out through the posteromedial portal. A sliding knot (fishing knot type) is applied to the most posterior part of the meniscus with the help of a knot pusher and then cut. The sutures are repeated as required depending on the length of the tear (usually we place a knot every 5 mm of the tear). During suturing, care must be taken to not splinter the meniscus that can occur with multiple failed attempts to pass the curved hook. Additionally, entangling of the sutures must be avoided. In some patients, the tear may extend to the mid-portion of the meniscus requiring further repair through the standard anterior portal with meniscal suture anchor and/or an outside-in suture. The stability of the suture is then tested with the probe.
Post-operative
Post operatively, active and passive range of motion is limited to 0-90º in the first six weeks. Full weight bearing is allowed by six weeks post-operatively. Jogging is permitted after 4 months, pivoting activity at 6 months, and unrestricted activities by 9 months.
Results
Ahn et al (4) in 140 patients showed complete healing in 118, incomplete healing in 17 and failure 5 repairs. The clinical success rate was 96.4% (135 of 140). Healing was associated with the type of tear and location. Incomplete healing and failures had complex tears or tears involving the red-white zone. Seventeen patients had incomplete healing at second-look arthroscopy but had no clinical sign of a meniscal tear. The mean Lysholm score and HSS scores improved post surgery (Table. 1) and 134 (95.7 %) patients had a normal (104 patients, 74.3%) or nearly normal (30 patients, 21.4%) the objective IKDC scores. In our prospective evaluation (46) of 132 patients undergoing a MM repair through a posteromedial portal in conjunction with ACL reconstruction, fifteen patients were found to be symptomatic according to Barret’s criteria on follow-up (6). The clinical failure rate was 9%, 4.9% in the subgroup “limited tear” and 15.7% in the subgroup “extended tear.” A limited tear was defined as one restricted to the posterior segment whereas those with a tear that extended to the mid-portion of the meniscus were classified as an extended tear. The extended tears required an additional repair through the standard anterior portal with meniscal suture anchor and/or an outside-in suture. The extended lesions had an increased risk of clinical failure. Out of the fifteen, 9 patients underwent revision surgery. Nine patients (6.8%) had failure of the meniscal repair; 3.7% (3/81) occurred in the subgroup of limited tears and 11.7% (6/51) in the subgroup extended tears. In the subgroup of extended tears, the cumulative survival rate did not decrease significantly and were not associated with a significant increased risk of revision of the MM. The average subjective IKDC improved at last follow-up and The Tegner activity scale at the last follow-up was slightly lower than before surgery (Table. 1).
Complications
The main complications may be related to the posteromedial portal placement. Damage to the infra-patellar branch of the saphenous nerve due to a posteromedial portal has been reported owing to the proximity of the nerve to the portal site causing hypoesthesia or paresthesia below the patella (27). Having said that, hypoesthesia resulting from harvesting the Semi-tendinous and Gracilis tendons in a concomitant ACL reconstruction may be responsible for 74% of the times (35). Transient hypoesthesia of the Sartorial branch of the saphenous nerve has also been reported probably due to an access portal situated too anteriorly (24). McGinnis et al (23) studied the neurovascular safety zone for the posteromedial access and recommended a portal through the posterior soft spot located formed by the medial head of the gastrocnemius, the tendon of the semimembranosus and the medial collateral ligament at the posterior aspect of the joint line for creation of the posteromedial portal. Hemarthrosis due to the long saphenous vein injury may occur in the postero medial approach (27). Among other complications, an iatrogenic medial meniscus tear may occur from repeated attempts at suturing the meniscus with a curved hook, rending suture impossible. Also, to our knowledge no popliteal artery, common peroneal and tibial nerve lesions has been reported, however they are at risk of damage during creation of the posterior portals. These complications may be avoided by placing the posterior portals with knee in 90 degrees of flexion. This moves the neurovascular structures posteriorly, away from the posteromedial portal site. Also, the Guillquist maneuver that provides trans-illumination may help visualize the course of the superficial veins and the accompanying nerves thus preventing inadvertent damage (35). Our series (46) also has a low complications rate with only two cases of hemarthrosis post operatively. Also, no patient developed a neuroma around the location of the posteromedial approach, although it was difficult to be accurately determining the incidence of saphenous nerve lesions due to the posteromedial approach as the hamstring tendon harvesting can cause hypoesthesia in the different territories of the saphenous nerve.
Discussion
The forces acting on the MM increase by as much as 200% after an ACL injury. Furthermore, forces acting on the ACL replacement graft increase by 33% to 50% after a medial meniscectomy (12,28). Deficiency of the medial meniscus has therefore been proposed as a secondary cause of ACL failure. It has thus been recommended that an ACL-deficient knee be reconstructed to protect the menisci (39,50). Conversely, identification and repair of a ramp lesion during an ACL reconstruction is imperative to reduce the risk of secondary graft failures, as these lesions may increase the anterior tibial translation (2,12, 30) and subsequently the strain on the graft. The success rates for meniscal repairs have been reported to be from 70% to 90% in vascular regions (11,13,16,36). Anh et al (12) reported a clinical successful healing rate of 96.4% in PHMM repairs with concomitant ACL reconstruction. Tenuta and Arciero (45) reported higher healing rates in concomitant ACL reconstruction than for isolated repairs (90% vs 57%). Meniscal repair in conjunction with ACL reconstruction has been reported to create a favorable environment for meniscal healing because of fibrin clot formation associated with intra-articular bleeding generated during ACL reconstruction (44). Multiple techniques for suturing the meniscus are available. The indications, advantages and disadvantages of each are mentioned in (Table.2). The all-inside suture repair technique using a hook is especially useful in a ramp lesion, as the use of newer devices makes the repair procedure blind and placing a suture in the vertical configuration is technically challenging. In addition Choi et al reported that the use of meniscal devices failed to provide sufficient strength of fixation. They recommended that during suturing, the posteromedial capsule should be elevated and approximated to the PHMM to ensure precise approximation of tear site (10). In spite of the development of the newer all-inside suture devices, the failure rate of the repair of PHMM tears continues to remains high, (19) which may be attributed to various factors that include inadequate visualization and debridement of the lesions of the PHMM; failure to confirm the reduction of the lesion with the all inside technique (48) and tissue failure due suture pullout through the meniscal tissue (45).
The mechanical strength of the vertical suture is greater than that of the horizontal suture (45). Having said that, most meniscal fixators cannot facilitate meniscal repair in a vertical mattress fashion (7,34) especially in the posteromedial corner of the medial meniscus, small or tight knee joints. Sutures spaced at every 3 to 5 mm have been recommended however; the optimal number is unknown (44). Pujol et al (33) using meniscal devices reported an overall healing rate of 73.1%. van Trommel et al (47) reported similar results (76%) with the outside-in technique. (Table. 3) Both studies observed a strong trend toward a relatively lower healing rate of the posterior horn (Zone A), as compared with the body (Zone B). (Table. 4) They also observed that, partial healing in all tears extending from the posterior to the middle third of the medial meniscus. We observed similar results in our study with a higher failure rate in the extended tear subgroup (6/51) (46). Pujol et al (33) attributed this to the difficulty in performing an adequate abrasion of the posterior segment using standard anterior arthroscopic portals whereas van Trommel et al (47) attributed that same to the relatively anterior placement of the needles with the outside-in technique, making a perpendicular repair extremely difficult. This resulted in a decrease in the coaptation force of the sutures. In addition, they observed that an oblique suture placement in the posterior zone with the outside-in technique made the sutures enter more anterior than they exit. Ahn et al (5) postulated that a torn posterior menisco-capsular structure moved inferiorly against the remaining meniscus, displacing the tear during knee flexion. They suggested that this motion of the torn medial meniscus can partially explain the slow healing observed in MMPH peripheral rim tears despite a rich vascular supply to the red-red zone. Pujol et al (31) in 2011 reported a secondary meniscectomy rate of 12.5%. The authors observed that the volume of meniscus removed decreased in 35% of cases, with respect to the initial tear and noted that a secondary meniscectomy following repair can partially save the meniscus and the failure called a ‘‘partial’’ failure. They recommended that suturing a tear therefore preserved the meniscal volume in a subsequent meniscectomy performed for a failure of repair or repeat tears. Tachibana et al (44) reported newly formed meniscal tears occurring in an area different from the initial repair site, on the surface of 34.5% of the healed and incompletely healed menisci. These new injuries were 1 to 3 mm in length partial- or full-thickness lesions and located central to the peripheral repair. In our series (46), the high rate of recurrent tear was as a result of newly formed tears that were confirmed on the surface of 5 menisci. It is conceivable that these injuries were attributable to a residual cleft left by the path of the Suture Lasso and maintained by the use of a strong no. 2 non-absorbable suture.
These clefts on the avascular meniscal substance may remain in situ without healing and would favor the recurrence of a more centrally located lesion in the white-white zone. Using a small suture hook device may therefore be desirable as it may reduce the size of the clefts created during suturing. In addition, the ‘cheese wiring effect’ due to the higher co-efficient of friction of a non-absorbable suture may contribute to a failure. We therefore decided to change our suture from a strong non-absorbable suture to a number 0 or 1 PDS suture, which are recommended to reduce the risk of these newly formed injury (37).
Nepple et al (26) observed that the time between injury and repair was the most important factor influencing healing. The zone of tear in reference to blood supply is another major factor affecting the results of a meniscal repair and ramp lesions in the red-red zone are expected to heal more readily than are those in the red-white zone (20). The criteria for healing based on follow-up arthro-CT corresponding to thickness of healing was suggested by Henning et al (36) can supplement clinical evaluation to improve diagnostic accuracy (Figure 3). The clinical failure rate in a systematic review ranged from 0% to 43.5%, with a mean failure rate of 15% (22). Failures after two years represented nearly 30% (26). Although numerous studies have reported short-term outcomes of various techniques of meniscal repair, relatively few have reported medium to long-term outcomes. The rate of meniscal repair failure appears to increase from short-term follow-up to medium to long-term follow-up regardless of the technique (26). There are limited numbers of studies assessing the outcomes of meniscal repair using the PM approach (4,5,10,46). Further prospective analysis with long – term follow-up is required to validate the promising early results of meniscal repairs performed with this approach. Finally, improved visualization is the key to achieving good meniscal repair results as it improves diagnosis of longitudinal tears in posterior horn MM (30), safeguards better debridement prior to repair and ensures good approximation of the torn ends under vision (1). It is thus important to perform a systematic exploration of the knee during an ACL reconstruction (Figure 1). A transnotch visualization combined with palpation of the meniscus with a needle or probe through the postero-medial portal aids in diagnosis of ramp lesions, which may otherwise be missed. Hidden lesions furthermore may be either very peripheral, covered by a layer of synovial or scar tissue or may not be reachable with a probe. It is therefore essential to identify these lesions during an ACL reconstruction and repair them whenever they are found to be unstable (40).
Conclusions
A systematic posteromedial exploration allows discovery of and debridement of the hidden MM lesion and repair with a suture hook device is associated with low morbidity. Failure Rates following a ramp lesion repair are low and occurs during the first 20 months. Even if a failure occurs the subsequent meniscectomy is limited and the volume of meniscal tissue debrided is reduced. An arthroscopic repair of meniscal ramp lesions should therefore be undertaken whenever possible.
References
1. Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register A Report on Baseline Variables and Outcomes of Surgery for Almost 18,000 Patients. The American journal of sports medicine. 2012 Oct 1;40(10):2230-5.
2. Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal Tear of the Medial Meniscus Posterior Horn in the Anterior Cruciate Ligament–Deficient Knee Significantly Influences Anterior Stability. The American journal of sports medicine. 2011 Oct 1;39(10):2187-93.
3. Ahn JH, Kim SH, Yoo JC, Wang JH. All-inside suture technique using two posteromedial portals in a medial meniscus posterior horn tear. Arthroscopy. 2004;20:101-108.
4. Ahn JH, Lee YS, Yoo JC, Chang MJ, Koh KH, Kim MH. Clinical and second-Look arthroscopic evaluation of repaired medial meniscus in anterior cruciate ligament–reconstructed knees. The American journal of sports medicine. 2010 Mar 1;38(3):472-7.
5. Ahn JH, Wang JH, Yoo JC. Arthroscopic all-inside suture repair of medial meniscus lesion in anterior cruciate ligament-deficient knees: results of second-look arthroscopies in 39 cases. Arthroscopy. 2004;20(9):936-45.
6. Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy 1998;14:824-829.
7. Boenisch UW, Faber KJ, Ciarelli M, Steadman JR, Arnoczky SP. Pull-out strength and stiffness of meniscal repair using absorbable arrows or Ti-Cron vertical and horizontal loop sutures. The American journal of sports medicine. 1999 Sep 1;27(5):626-31.
8. Bollen SR. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognized association. J Bone Joint Surg Br. 2010;92:222-223.
9. Bonnin M, Carret JP, Dimnet J, Dejour H. The weight-bearing knee after anterior cruciate ligament rupture: an in vitro biomechanical study. Knee Surg Sports Traumatol Arthrosc. 1996;3:245-251.
10. Choi NH, Kim TH, Victoroff BN. Comparison of Arthroscopic Medial Meniscal Suture Repair Techniques Inside-Out Versus All-Inside Repair. The American journal of sports medicine. 2009 Nov 1;37(11):2144-50.
11. DeHaven KE. Meniscus repair. The American journal of sports medicine. 1999;27:242-250.
12. Edgar C Hartford W, Ware, Obopilwe, E Ziegler C, Reed D, Arciero R. Posteromedial Meniscocapsular Tear: Prevalence, Detection Sensitivity, Biomechanics, and Repair Technique. Scientific Exhibit SE81. AAOS 2015.
13. Feng H, Hong L, Geng XS, Zhang H, Wang XS, Jiang XY. Secondlook arthroscopic evaluation of bucket-handle meniscus tear repairs with anterior cruciate ligament reconstruction: 67 consecutive cases. Arthroscopy. 2008;24:1358-1366.
14. Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Intraoperative findings and procedures in culturally and geographically different patient and surgeon populations: an anterior cruciate ligament reconstruction registry comparison between Norway and the USA. Acta Orthop. 2012;83:577-582.
15. Hamberg P, Gillquist J, Lysholm JA. Suture of new and old peripheral meniscus tears. J Bone Joint Surg Am. 1983 Feb 1;65(2):193-7.[9]
16. Henning CE. Current status of meniscus salvage. Clin Sports Med. 1990;9:567-576.
17. Ihara H, Miwa M, Takayanagi K, Nakayama A. Acute torn meniscus combined with acute cruciate ligament injury: second look arthroscopy after 3-month conservative treatment. Clin Orthop Relat Res. 1994;307:146-154.
18. Kaplan PA, Walker CW, Kilcoyne RF, Brown DE, Tusek D, Dussault RG. Occult fracture patterns of the knee associated with anterior cruciate ligament tears: assessment with MR imaging. Radiology. 1992;183(3):835-838.
19. Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy. 2006;22(1):3-9.
20. Krych AJ, McIntoch AL, Voll AE, Stuart MJ, Dahm DL. Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med. 2008;36:1283-1289.
21. Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. The American journal of sports medicine. 2011;39:832-837.
22. Lozano J, Ma CB, Cannon WD. All-inside meniscus repair: a systematic review. Clin Orthop Relat Res. 2007;455:134-141.
23. McGinnis MD, Gonzalez R, Nyland J, Caborn DN. The posteromedial knee arthroscopy portal: a cadaveric study defining a safety zone for portal placement. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2011 Aug 31;27(8):1090-5.
24. Morgan CD, Casscells SW. Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1986 Dec 31;2(1):3-12.
25. Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. The American journal of sports medicine. 1991 Dec 1;19(6):632-8.
26. Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012 Dec 19;94(24):2222-7.
27. Ogilvie-Harris DJ, Biggs DJ, Mackay M, Weisleder L. Posterior portals for arthroscopic surgery of the knee. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1994 Dec 31;10(6):608-13.
28. Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29:226-231.
29. Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H. Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:1438-1444.
30. Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surgery, Sports Traumatology, Arthroscopy. 2015 Oct 1;23(10):2967-73.
31. Pujol N, Barbier O, Boisrenoult P, Beaufils P. Amount of meniscal resection after failed meniscal repair. The American journal of sports medicine. 2011 Aug 1;39(8):1648-52.
32. Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17:396-401.
33. Pujol N, Panarella L, Selmi TA, Neyret P, Fithian D, Beaufils P. Meniscal Healing After Meniscal Repair A CT Arthrography Assessment. The American journal of sports medicine. 2008 Aug 1;36(8):1489-95.
34. Rankin CC, Lintner DM, Noble PC, Paravic V, Greer E. A biomechanical analysis of meniscal repair techniques. Am J Sports Med. 2002;30:492-497.
35. Sanders B, Rolf R, McClelland W, Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: an anatomic and clinical study of sartorial branch injury. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2007 Sep 30;23(9):956-63.
36. Scott GA, Jolly BL, Henning CE. Combined posterior incision and arthroscopic intra-articular repair of the meniscus: an examination of factors affecting healing. J Bone Joint Surg Am. 1986;68: 847-861.
37. Seil R, Rupp S, Jurecka C, Rein R, Kohn D. Effect of various suture strength factors on behavior of meniscus sutures in cyclic loading conditions. Unfallchirurg 2001;104:392-398.
38. Seil R, VanGiffen N, Pape D. Thirty years of arthroscopic meniscal suture: what’s left to be done? Orthop Traumatol Surg Res. 2009;95:S85-S96.
39. Shoemaker SC, Markolf KL. The role of the meniscus in the anteriorposterior stability of the loaded anterior cruciate-deficient knee: effects of partial versus total excision. J Bone Joint Surg Am. 1986;68:71-79.
40. Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden Lesions of the Posterior Horn of the Medial Meniscus A Systematic Arthroscopic Exploration of the Concealed Portion of the Knee. The American journal of sports medicine. 2014 Feb 24:0363546514522394.
41. Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial Meniscocapsular Lesions Increase Tibiofemoral Joint Laxity With Anterior Cruciate Ligament Deficiency, and Their Repair Reduces Laxity. Am J Sports Med. 2016 Feb;44(2):400-8. doi: 10.1177/0363546515617454. Epub 2015 Dec 11.
42. Strobel MJ. Menisci. In: Fett HM, Flechtner P, eds. Manual of Arthroscopic Surgery. New York: Springer; 1988:171-178.
43. Sullivan D, Levy IM, Sheskier S, Torzilli PA, Warren RF. Medial restraints to anterior-posterior motion of the knee. J Bone Joint Surg Am. 1984;66:930-936.
44. Tachibana Y, Sakaguchi K, Goto T, Oda H, Yamazaki K, Iida S. Repair integrity evaluated by second-look arthroscopy after arthroscopic meniscal repair with the FasT-Fix during anterior cruciate ligament reconstruction. The American journal of sports medicine. 2010 May 1;38(5):965-71.
45. Tenuta JJ, Arciero RA. Arthroscopic evaluation of meniscal repairs: factors that effect healing. Am J Sports Med. 1994;22:797-802.
46. Thaunat M, Jan N, Fayard JM, Kajetanek C, Murphy CG, Pupim B, Gardon R, Sonnery-Cottet B. Repair of Meniscal Ramp Lesions Through a Posteromedial Portal During Anterior Cruciate Ligament Reconstruction: Outcome Study With a Minimum 2-Year Follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016 May 13.
47. van Trommel MF, Simonian PT, Potter HG, Wickiewicz TL. Different regional healing rates with the outside-in technique for meniscal repair. The American journal of sports medicine. 1998 May 1;26(3):446-52.
48. Walgrave S, Claes S, Bellemans J. High incidence of intraoperative anchorage failure in FasT fix all inside meniscal suturing device. Acta Orthop Belg. 2013;79(6):689-93.
49. Warren RF, Marshall JL. Injuries of the anterior cruciate and medial collateral ligaments of the knee: a long-term follow-up of 86 cases– part II. Clin Orthop Relat Res. 1978;136:198-211.
50. Yoo JC, Ahn JH, Lee SH, Yoon YC. Increasing incidence of medial meniscal tears in nonoperatively treated anterior cruciate ligament insufficiency patients documented by serial magnetic resonance imaging studies. Am J Sports Med. 2009;37:1478-1483.
(Abstract) (Full Text HTML) (Download PDF)
Inside-Out Meniscus Repair – A Review
Sachin Ramchandra Tapasvi, Anshu Shekhar, Shantanu Sudhakar Patil
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 14-18
Author: Sachin Ramchandra Tapasvi [1], Anshu Shekhar [1], Shantanu Sudhakar Patil [1]
[1] The Orthopaedic Specialty Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004.
Address of Correspondence
Dr Sachin Ramchandra Tapasvi
The Orthopaedic Speciality Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004
Email: stapasvi@gmail.com
Abstract
Meniscus tears are common knee injuries presenting to an arthroscopy surgeon. Repairing the meniscus to salvage knee function and biomechanics is indicated where ever possible, since the problems after meniscectomy are well established now. Inside-out meniscus repair is a very useful technique to repair tears in the posterior and middle third of both menisci. Proper adherence to technique and safety incisions reduce the risks and complications to almost the level of an all-inside meniscus repair. The technique allows precise placement of sutures, causes minimal meniscus tissue trauma, has produced good healing rates, is cost-effective and is basically, an indispensable tool in the armamentarium of any knee surgeon.
Key Words: Meniscus, Meniscus repair, Inside-out, Safety incision, Complications.
Introduction
Once considered expendable, the vital role of meniscus in knee biomechanics is firmly established now. They are known for contributing to knee stability and congruity, resisting capsular and synovial impingement, load distribution and contribution towards screw home mechanism[1]. With advances in arthroscopy in terms of technique, instrumentation, optics and biomaterials, meniscus salvage has become a thrust area in this field today. The three basic techniques of meniscus repair: outside-in, inside-out and all-inside each have their indications, advantages and pitfalls. Henning et al first described the inside-out technique of meniscus repair, involving meniscal and meniscosynovial abrasion to promote healing, cannulated suture-needle delivery system for suture placement, a posteromedial or lateral skin incision for suture needle retrieval[2]. Here, we review the inside-out technique of meniscus repair.
Indications For Inside-out Repair And Technique
A meniscus tear must first be deemed suitable for repair, before deciding on the technique to be used. A non-degenerated, longitudinal tear, less than 3 centimeter and in the peripheral vascular zone is most amenable to repair[3]. An inside-out meniscus repair can be performed for the mid-third and posterior-third longitudinal tear of both the menisci[4]. With advances in all-inside meniscus repair implants and technique, this has gradually become the standard method of repair for posterior third longitudinal meniscus tears, replacing the “gold standard” method of inside-out repair[5]. Middle third tears, however, are readily amenable to repair by the inside-out technique without significant risk to neurovascular structures and possibly, without the need for a safety incision. Radial tears repaired by an all-inside or an inside-out horizontal construct have similar maximum failure loads [6]. The most recent systematic review comparing all-inside with inside-out isolated meniscus repairs did not reveal any difference in the failure rates, functional outcomes, and complications between the two methods[7]. However, the inside-out techniques has some distinct advantages. The zone specific suture needle delivery cannulae facilitate more precise and controlled suture placement, while allowing for revision and improvisation[8]. Also, the finer needles cause less iatrogenic damage to meniscus tissue, compared with the heavier all-inside implant insertion needles. This is especially vital when the meniscus tissue is tenuous, or in case of a complex tear. The finer needles also provide greater number of fixation points and captures more collagen tissue[8]. Another important advantage of inside-out repair technique is the significant savings in terms of implant cost of expensive all-inside repair devices [8].
Surgical technique
Patient position for inside-out meniscus repair can be either with a leg holder and table broken or on a flat table with thigh side support. A proximal thigh tourniquet is used for good visualization. A diagnostic arthroscopy is first performed via an anterolateral portal. A high anterolateral portal is useful if a meniscus repair is planned, to allow the needles to pass over the tibial spines without struggle. The anteromedial portal is created under vision with the aid of a spinal needle to allow easy access to medial and lateral menisci[8]. Typically, for a lateral meniscus repair, the anteromedial portal is higher to allow needles to negotiate the tibial spine[9].
A 70 degree scope placed through the notch is helpful in viewing far posterior tears[9]. Assessment of the tear is done to decide whether to proceed with a repair or to resect the meniscus. Preparation of the meniscus tear is done next to potentiate healing. Granulation tissue must be debrided from both sides of the meniscus tear. Abrading the meniscal and peri-meniscal synovium, both superiorly and inferiorly, with a meniscus rasp (Acufex, Andover, MA) is an useful augment and aids in healing response[10]. Trephination is believed to create vascular channels and increase blood flow from a more vascular to a less vascular area[11][12]. A useful trick in bucket handle tears is to prepare the edges of the tear while the meniscus is still displaced and access to both sides is easy[8] (Figure 1). Fibrin clot prepared from the patient’s own blood is also widely used to enhance healing. It not only provides a scaffold, but also acts as an initiator and activator of the healing process[13]. When a meniscus repair is being performed in isolation, performing a limited notchplasty of the lateral femoral condyle with a shaver to create postoperative hemarthrosis and deliver marrow elements is another method of biological augmentation[9].
A. Technique for Medial meniscus inside-out repair[9]:
A 3-4 centimeter vertical “safety incision” (Figure 2) in the posteromedial aspect of the joint, posterior to the medial collateral ligament is first made with the knee in 60-900 flexion, to relax the hamstrings and popliteal neurovascular bundle. Transillumination aids in precise placement of this incision, with two-thirds being distal to the joint line and one-third proximal to it. The saphenous vein is carefully protected and sartorius fascia is incised and split proximally and distally with Metzenbaum scissors to preserve the Sartorius, Gracilis, Semitendinosus and the Saphenous nerve, which lies posterior to the Sartorius. Deep dissection is carried out bluntly with Metzenbaum scissors to create a plane between the medial head of gastrocnemius and capsule. This dissection is better performed from distal to proximal. Dorsiflexion and plantar flexion of the foot aids is location of the proper plane. A Henning retractor or a small bent spoon is then inserted anterior to the gastrocnemius, which protects the popliteal neurovascular bundle, retracts the pes and gastrocnemius and deflects the needle medially for retrieval. Repair can then begin, starting posteriorly and working anteriorly, with the knee in 10-200 flexion. Visualization of posterior meniscus can be improved by pie-crusting of the medial collateral ligament just below the joint line, while applying a valgus-external rotation force. Zone specific single and double lumen cannulae (Acufex, Andover, MA) inserted from the anterolateral portal are used to keep the meniscus reduced and for precise placement of the needles. For tears very close to the posterior root, it might become necessary to insert a curved cannula from the anteromedial portal, the curvature being directed away from the midline, to achieve proper trajectory for the suture needle. Non-absorbable multi-strand, long chain ultra-high molecular weight polyethylene (UHMWPE) sutures on 10 inch long needles (No. 2-0 FiberWire, Arthrex, Naples, FL) are used for the repair. The cannula is retracted 3-5 mm when the needle is pierced to increase the accuracy. This is done for the femoral side first, attempting to achieve a vertical mattress configuration, as this provides greater capture of strong circumferential fibers of the meniscus[8] (Figure 3).
This might create a puckering of the meniscus, which subsides when tibial sided sutures are passed in a similar fashion to create a stacked repair and provide better coaptation of the tear area[14] (Figure 4). The needles are passed by one assistant, while a second assistant retrieves them using a needle driver, clips it using a hemostat and cuts the needles, taking care to avoid needle stick injury to anybody. If the needle is not visible after passing 1-1.5 centimeter, it must be withdrawn and reinserted at the same or different location with a different trajectory. Multiple sutures maybe passed at 3-5 mm intervals. The sutures may be tied sequentially as they are passed or at the end, after all have been passed out. When tying the knots, the knee must be kept in near or full extension to avoid imbricating the capsule, effectively causing a capsulorrhaphy and consequent flexion contracture. Drains may or may not be used and closure of the safety incision is done in layers.
B. Technique for Lateral meniscus inside-out repair[9]:
The general principles remain the same as for a medial meniscus repair, with some important differences. The lateral vertical safety incision is made in a similar fashion, posterior to the fibular collateral ligament, two-thirds distal and one-third proximal to the joint line. The interval between biceps femoris and iliotibial band is dissected bluntly with a pair of Metzenbaum scissors, the common peroneal nerve being posteromedial to the biceps tendon (Figure 5). Dissection between the lateral gastrocnemius head and posterolateral capsule is similarly begun distally and a finger is used to assess the proper plane by flexing and extending the ankle. Staying anterior to the biceps and gastrocnemius lateral head reliably protects the common peroneal nerve A Henning retractor or bent spoon is placed as for the medial side, between the capsule and gastrocnemius. The anteromedial portal is made higher to avoid the eminence of the tibial spine, under vision over a spinal needle with the knee in a figure-of-4 position. If need be, accessory high anteromedial portal can be made to improve suture needle trajectory. The cannula is never inserted from the anterolateral portal due to the potential risk to the popliteal vessels, which lie just posterior to the posterior horn of the meniscus. Though no problems have been reported, it is best to avoid the popliteus tendon and pass sutures adjacent to this structure[9]. Capsular capture is not a problem on the lateral side and hence, knot tying can be done with the knee in flexion.
Discussion
Result
The inside-out repair technique offers a success rate of 60% to 80% for isolated meniscus repairs and between 85% and 90% when performed with a concomitant ACL reconstruction[5]. Horibe et al performed second look arthroscopy for 132 meniscus repairs by inside-out technique. They report 74% excellent (completely healed) and 17% good (incomplete healing, partial thickness defect, stable on probing) result in their cohort[14]. Choi et al compared the results of suture repair of meniscus tears with concomitant ACL reconstruction, by all-inside and inside-out techniques using polydioxanone sutures. They found no difference in the healing rates on magnetic resonance imaging and no difference in Lysholm scores or Tegner activity scales between the two groups[15]. A systematic review by Grant et al was done to compare the effectiveness and complications of isolated inside-out and all-inside meniscus repairs. There was no statistical difference in clinical failure rate- 17% for all-inside and 19% for inside-out techniques. Subjective outcome, as measured by Lysholm score and Tegner activity scale was also comparable between the two groups. Inside-out repairs however, require 50% greater operative time. Nerve related symptoms were commoner (9%) in the inside-out group than in the all-inside group(2%). Upon pooling of all complication data, the Odd’s ratio was 0.55 (95% confidence interval = 0.27, 1.10). 0.55 (95% confidence interval = 0.27, 1.10)[16]. In a more recent systematic review, Fillingham et al compared current all-inside repair devices with the classical inside-out repair for isolated meniscus tears. They reported no significant differences in clinical or anatomic failure rates (clinical failure: 11% for inside-out versus 10% for all-inside, respectively, p=.58; anatomic failure: 13% for inside-out versus 16% for all-inside repairs, p=.63). Mean ± SD Lysholm score and Tegner score for inside-out repair were 88.0 ± 3.5 and 5.3 ± 1.2, while the respective scores for all-inside repair were 90.4 ± 3.7 and 6.3 ± 1.3. Complications occurred at a rate of 5.1% for inside-out repairs compared to 4.6% for all-inside repairs[7].
Complications and Problems:
The various anatomic structures in the needle trajectory can potentially be injured. By deploying safe surgical practices, they can be avoided. These are some of the commonly encountered problems:
1. Saphenous nerve injury- It can be avoided by the medial safety incision and keeping the nerve, which lies posterior to the Sartorius, retracted behind the pes tendons.
2. Common peroneal nerve injury- The nerve lies posteromedial to the biceps femoris. Injury is avoided by keeping the knee in flexion while making the lateral skin incision and carefully developing the plane between the biceps femoris and iliotibial band.
3. Popliteal vessels- are most at risk while doing a posterior lateral meniscus repair. Careful placement of retractor and always passing suture needles from the anteromedial portal with careful retrieval, avoids injury to the vessels.
4. Flexion contracture may develop- when the medial side sutures are tied with the knee in flexion, thus over tightening the posteromedial capsule.
5. Needle stick injury to the surgeon or assistants- avoided by careful, unhurried movements[8].
The inside-out technique also has an increased operative time, compared to all-inside technique by about 50%[16].
Conclusions
The inside-out method of meniscus repair is an excellent technique to repair tears in the middle and posterior-third of both menisci. With the rapid development of all-inside meniscus repair devices, this technique may not remain the “gold standard” but still has an important role, especially in repairing large and complex tears. When care is taken to protect the neurovascular structures posteriorly, and with due diligence to correct surgical technique, it is a safe, cost effective and proven method to salvage the menisci whenever possible.
References
1. Renstrom P, Johnson RJ. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990 Jul;9(3):523-38.
2. Henning CE. Arthroscopic repair of meniscus tears. Orthopedics 1983; 6: 1130–1132.
3. Taylor S.A., Rodeo S.A. Augmentation techniques for isolated meniscal tears. Curr Rev Musculoskelet Med. 2013 Jun; 6(2): 95–101.
4. Yoon KH, Park KH. Meniscal Repair. Knee Surg Relat Res. 2014;26(2):68-76
5. Turman KA, Diduch DR. Meniscal repair: indications and techniques. J Knee Surg. 2008 Apr;21(2):154-62.
6. Branch EA, Milchteim C, Aspey BS, Liu W, Saliman JD, Anz AW. Biomechanical comparison of arthroscopic repair constructs for radial tears of the meniscus. Am J Sports Med. 2015 Sep;43(9):2270-6
7. Fillingham YA, Riboh JC, Erickson BJ, Bach BR Jr, Yanke AB. Inside-Out Versus All-Inside Repair of Isolated Meniscal Tears: An Updated Systematic Review. Am J Sports Med. 2016 Mar 17. pii: 0363546516632504. [Epub ahead of print]
8. Nelson C.G., Bonner K.F. Inside-out meniscus repair. Arthrosc Tech. 2013 Nov; 2(4): e453–e460.
9. Bonner KF. Meniscus repair: Inside-out suture technique. In: Jackson DW, editor. Master techniques in orthopaedic surgery: Reconstructive knee surgery. Ed 3. Philadelphia: Lippincott, Williams & Wilkins; 2008:71-88.
10. Ritchie JR, Miller MD, Bents RT, Smith DK. Meniscal repair inthe goat model. The use of healing adjuncts on central tears and the role of magnetic resonance arthrography in repair evaluation. Am J Sports Med. 1998;26:278–84.
11. Zhang Z, Arnold JA, Williams T, McCann B. Repairs by trephination and suturing of longitudinal injuries in the avascular area of the meniscus in goats. Am J Sports Med. 1995;23:35–41.
12. Fox JM, Rintz KG, Ferkel RD. Trephination of incomplete meniscal tears. Arthroscopy. 1993;9:451–5.
13. Ra HJ, Ha JK, Jang SH, Lee DW, Kim JG. Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc. 2013;21:2126–2130
14. Horibe S, Shino K, Maeda A, Nakamura N, Matsumoto N, Ochi T. Results of isolated meniscal repair evaluated by second-look arthroscopy. Arthroscopy. 1996;12(2):150-155
15. Choi NH, Kim TH, Victoroff BN. Comparison of arthroscopic medial meniscal suture repair techniques: Inside out versus all-inside repair. Am J Sports Med 2009;37:2144-2150.
16. Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: A systematic review. Am J Sports Med 2012;40:459-468.
(Abstract) (Full Text HTML) (Download PDF)
All-Inside Meniscus Repair
William M Weiss, F. Alan Barber
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 8-13
Author: William M Weiss[1], F. Alan Barber[2]
[1] Texas Tech University Health Sciences Center El Paso, Texas.
[2[ Plano Orthopedic Sports Medicine and Spine Center Plano, Texas.
Address of Correspondence
Dr William M Weiss
Texas Tech University Health Sciences Center Department of Orthopedic Surgery and Rehabilitation 4801 Alberta Avenue El Paso, Texas 79902.
E-mail: william.m.weiss@ttuhsc.edu
Abstract
Meniscal surgery has undergone a considerable shift in goals over the last century. While early meniscal surgery consisted of mostly total meniscectomy, recognition of the importance of this structure resulted in a shift to partial meniscectomy, and then to repair in appropriate patients. The over-reaching goal is now the preservation of meniscal tissue to minimize the risk of osteoarthritis, particularly in the young athlete. Technologic advances in arthroscopy and instrumentation have allowed the development of minimally invasive techniques, which decrease the risks associated with open surgery. While no meniscal repair technique has been demonstrated to be superior in its outcomes, the all-inside technique requires no accessory incisions and minimizes the risk to posterior structures. While the early all-inside implants have been shown to risk chondral damage, the literature demonstrates that newer suture-based implants do not share these complications, and result in the healing of appropriate tears.
Key Words: All-inside, Meniscal tear, Meniscal repair, Chondral injury.
Introduction
The first open meniscal repair was performed in 1885 [1], though resection has been more common. With the advent of arthroscopy, minimally invasive techniques replaced open repairs, and provided better access to difficult areas while minimizing surgical risks. The inside-out suture repair was initially the described, and continues to be used with excellent results [2]. The outside-in repair was developed later to decrease risk of injury to posterior neurovascular structures [3]. In recent years, advances in instrument and implant technology have allowed the development of all-inside repair techniques. These rely on specialized implants, but avoid additional incisions, decreasing risk to posterior neurovascular elements, and reducing surgical times [4]. The purpose of this review is to examine the evolution of the all-inside meniscal repair technique, with outcomes and complications.
Meniscus Anatomy, Function, And Healing:
The menisci are crescent shaped fibrocartilaginous structures situated in both the medial and lateral compartments of the knee, between the femur and tibia. Each meniscus has an anterior and posterior horn, and is attached to the tibia by the anterior and posterior meniscal roots and to the peripheral capsule by the coronary ligaments. They are triangular in cross section, conforming to both the distal femur and proximal tibia. This conformity effectively deepens the articular surfaces of the knee, providing shock absorption and contributing to stability, particularly with injury to stabilizing ligaments. This also increases the surface area for load distribution to the articular cartilage, decreasing contact stresses by converting vertical compression stresses to radially oriented hoop stresses [5, 6]. By maintaining space in the joint, the meniscus improves diffusion of synovial fluid, and provides nutrition and lubrication to the cartilage. The healing capacity of the meniscus is determined primarily by blood supply, as it is largely avascular and does not typically heal spontaneously. The meniscus is divided into zones in accordance with blood supply and healing capacity. The peripheral third (within 3 mm of the meniscosynovial junction) is well vascularized, as the blood supply enters the here [7]. This zone is referred to as red-red, and is mostly likely to heal. The inner third (over 5 mm from the meniscosynovial junction) receives no vascular supply, is called the white-white zone, and is least likely to heal. The middle zone, called red-white (between 3 to 5 mm from the meniscosynovial junction), has some vascularity [7, 8]. Red-red zone tears are commonly repaired in appropriate patients, while repairs of red-white zone tears are less likely to heal. Meniscal tear characteristics also influence healing potential. Longitudinal vertical tears (including bucket handle tears and meniscocapsular tears) have the capacity to heal with repair, while degenerative or complex (multi-planar), radial, horizontal, or flap tears are much less likely. Larger and less stable meniscal tears have higher failure rates, as have those repaired more than 8 weeks from injury [9]. Lateral compartment tears are also more likely to heal than those occurring medially [9]. This may be due to increased blood supply to the posterior horn of the lateral meniscus.
Meniscal Repair Technique
To overcome the inherent physiologic challenges of meniscal repair, the environment and technique must be optimized. Factors controlled by the surgeon include tissue preparation, the stability of fixation, knee stability and leg alignment, and post-operative rehabilitation. Preparation should include rasping of the tear, and the perimeniscal synovium. This stimulates the healing response [10], and can allow healing of isolated stable tears without fixation, particularly with concomitant ACL reconstruction [10,11]. Some advocate trephination to create vascular access channels, which may contribute to fibrovascular healing of avascular areas [12]. The addition of fibrin clot [13, 14], platelet-rich fibrin matrix [15], and collagen matrix with bone marrow [16] have been demonstrated to aid healing. Meniscal repair with associated ACL reconstruction improves healing, possibly by increasing blood in the joint, while lack of ACL function practically assures failure from stresses on the repair [17, 18]. ACL deficiency increased the failure rates of meniscal repair from 5% to 46% [19], demonstrating the importance of stability. Normal knee alignment also is required for successful meniscus repair outcomes. Forces within the knee, and through the meniscus, during normal gait can reach four times body weight and present significant challenges to fixation [20]. However, during unloaded knee motion the meniscus experiences only compressive forces [21, 22]. Therefore, fixation should maintain tissue approximation and neutralize sheer stresses. For suture-based repairs, vertically oriented non-absorbable sutures are considered the gold-standard, because of load to failure [23]. This configuration encircles the strong circumferential fibers, maximizing strength. Meniscus repairs are weak at the scar after 12 weeks 24, and visual evidence of healing at second-look arthroscopy has been seen at up to four months [25].
Surgical Technique Of Meniscus Fixation:
Arthroscopic techniques are the preferred method for meniscal repair; however no consensus exists as to the best technique. The most common indication for all-inside repair is tears of the posterior horn, as risk to neurovascular structures is decreased. All-inside repairs require less surgical time than other methods [26]. However, all-inside repairs do require an intact meniscal rim, highly specialized instruments, and implants. All-inside meniscal repair devices have progressed from rigid implants to current adjustable suture-based devices. Earlier versions of all-inside devices are no longer widely used or recommended. The adjustable suture-based all-inside devices are the state of the art.
Self-Adjusting Suture Containing Implants
The current generation of all-inside devices use ultra-high molecular weight polyethylene (UHMWPE) containing suture to connect typically non-absorbable poly ether-ether-ketone (PEEK) anchors. The suture is pre-tied, typically with a sliding and self-locking knot. Insertion instruments require only standard anterior portals, and often use a disposable cannula or a skid to aid passage. The meniscus repair device is inserted through the inner meniscus fragment to a pre-determined depth of the peripheral rim, often guided by the cannula. Once both anchors are deployed, the sliding-locking knot is cinched to compress the tear. This adjustability allows appropriate tensioning for reduction and healing, and the option to place horizontal, oblique, or vertical configurations.
The FasT-Fix (Smith & Nephew, Andover, MA) was the first adjustable suture-based device (Fig. 1). It consisted of two 5 mm anchors, made of either poly L lactic acid (PLLA, absorbable) or polyacetal (nonabsorbable) connected by No. 0 non-absorbable braided polyester suture. The anchors are delivered by an instrument that is either straight or angled 22°. Once both anchors span the tear, the pre-tied sliding-locking knot is tensioned using a knot pusher/suture cutter. The original design was modified to become the Ultra Fast-Fix by reconfiguring the needle to facilitate insertion, and replacing the suture with a stronger No. 0 UHMWPE UltraBraid. The current iteration is the FasT-Fix 360 (Fig. 2), in which the anchors have been reconfigured to PEEK with an arrow design, and the suture is now No. 2-0 UltraBraid.
The RapidLoc (Mitek, Raynham, MA) was an adjustable suture-based device, consisting of a PLLA “backstop” and a PLLA or polydioxanone (PDS) “top hat”, connected by either a No. 2-0 absorbable Panacryl or non-absorbable braided polyester suture (Fig. 3). The “backstop” anchor was placed across the tear to be extra-capsular, and the pre-tied sliding knot and “top hat” was then advanced, compressing the tear. The instrument included straight, 12° and 27° angled needles.
The OmniSpan (Mitek, Raynham, MA) replaced the RapidLoc, and uses a loop of No. 0 OrthoCord (55% PDS and 45% UHMWPE) suture between two PEEK anchors (Fig. 4). The sliding-locking knot is outside the loop, reinforcing the first anchor, and forming a double suture repair without a knot on the articular surface. Both loops of the repair are tightened concurrently, allowing equal tension. This device allows sutures to be placed in both horizontal and vertical mattress fashion.
The Meniscal Cinch (Arthrex, Naples, FL) has undergone incremental improvements since its inception (Fig. 5). The device is inserted with a 15° curved “gun” containing two separate trocar needles. It has an adjustable depth limiter on the handle, which is most commonly used at 18 mm. Each needle is loaded with a tubular PEEK anchor, and connected with a No. 2-0 FiberWire composed of UHMWPE and braided polyester (Arthrex Inc, Naples FL). The system includes a blue plastic “shoehorn” cannula to facilitate insertion, which is 6 mm in diameter and requires a large portal. The instrument allows placement of a vertical mattress stitch, secured with a pre-tied sliding-locking knot. After insertion, the first needle is removed and handed off. The second needle is “clicked” into position, and then a second device is inserted. Once both devices are deployed, the suture is gently pulled at the handle to tension the repair. A disposable knot pusher/suture cutter is provided.
The Sequent meniscal repair device (ConMed Linvatec, Largo, FL) utilizes No. 0 Hi-Fi (braided UHMWPE) suture with up to seven PEEK anchors measuring 1.3 mm in diameter and 5.1 mm long (Fig. 6). Each anchor is placed individually through the meniscus, with a straight or 15° curved instrument, and deployed on the extra-capsular surface. The suture is then tensioned to set the anchor into the tissue, and additional anchors can then be placed with the same device. A minimum of 3 anchors must be inserted to complete the repair, although more can be used to create an all-inside continuous stitch. This allows numerous stitch configurations, from continuous to interrupted stitches, and vertical or horizontal mattresses. This is the only device that can place multiple stitches without removal from within the joint. However, the technique is demanding, and practice in the laboratory prior to use is advised. The set includes a side-loading disposable suture cutter for use at completion.
The MaxFire MarXmen (Biomet Sports Medicine, Warsaw, Indiana) is an self-adjusting all-inside all-suture implant with No. 0 MaxBraid PE (UHMWPE) and two braided polyester sleeves serving as anchors (Fig. 7). It is similar to the JuggerKnot all-suture anchor in design and function, but modified for the meniscus. The instrument uses a needle (straight or curved) to insert the suture and two polyester anchors through the meniscus. The sliding-locking knot allows tensioning, and devices can be placed in either a horizontal or vertical mattress fashion.
The CrossFix meniscal repair system (Cayenne Medical, Scottsdale, AZ) passes a No. 0 Force Fiber (UHMWPE) suture through two parallel 15 gauge hollow needles (straight or curved 12°, Fig. 8). Once the needles penetrate the meniscus, crossing the tear, a small shuttle passes the suture from one needle to the other on the extra-capsular surface. As the needles are withdrawn, a 3 mm horizontal mattress suture is left, and a pre-tied sliding Weston knot is advanced to secure the reduction. Additional arthroscopic knots can be added as reinforcement, if desired.
The AS (all suture) Repair device (Covidien, Minneapolis, MN) is similar to the CrossFix in design and function (Fig. 9). While the two needles are the same size, the AS repair device has conical solid needles with a polymer coat (NuCoat) to facilitate penetration. The instrument can be straight or curved 15°, and passes a No. 2-0 UHMWPE suture using a similar shuttle needle, but uses a modified Tennessee slider knot with two half hitches to secure the repair. Both instruments result in a 3 mm wide horizontal mattress, with a knot on the meniscal surface that risks chondral injury. Due to the instrument dimensions, only horizontal mattress sutures are possible. Conceptually, this newest generation of all-inside suture based devices allows improved reduction, tissue compression, and stability compared to previous iterations. The overall goal of all-inside meniscal repair devices is to decrease complications seen with the earlier generations, and promote healing. However, these devices can generate significant tension which may be detrimental, leading to implant failure. Few investigations regarding outcomes and complications of these adjustable all-inside suture implants are available in the literature.
Results Of All-inside Meniscal Repair:
Arthroscopic meniscal repair methods have similar outcomes to open methods, with the gold standard inside-out suture repair having a success rate of 82% [17, 27], and outside-in suture repairs having success rates as high as 87% [28]. The original suture-based all-inside technique described by Morgan reported good results, but without any long term follow-up [29]. Early devices which rely on arthroscopic knot tying demonstrate up to 90% success initially, but this declines to 81% at 1 year [30].
Suture based implants have good strength, and are biomechanically equivalent to the gold standard vertical mattress sutures [31,32]. However, as this is the latest generation of all-inside devices, there is little long term outcome data available. The RapidLoc has demonstrated success rates of 86 to 91% [33, 34, 35], but there are reported failure rates of 35% [36] with complications reminiscent of rigid devices [37]. Longer term follow-up of these devices shows re-operation rates of 48% [38]. The FasT-Fix has also shown success rates from 82 to 92% [39,40], but with limited reports of complications. All-Inside devices have been demonstrated to have greater failure strength than inside out alternatives in the repair of radial meniscal tears [41].
Comparison Of Meniscal Repair Devices: Author’s preferred technique:
A human cadaver knee based comparison of several all-inside meniscus repair devices was carried out by the senior author to compare the technical ease, reproducibility, and consistency of using these devices in human meniscus tissue. A needle penetration depth limited to 18mm was found to be anatomically safe. Curved needles effectively reached the posterior horn with minimal articular cartilage injury. However, significant differences were observed in the technical ease, reproducibility, and consistency of all these devices. The FastFix 360 and OmniSpan were easiest to insert, least likely to excoriate articular cartilage, and most consistent in performance. Yet, the OmniSpan did not have any knot or device on the surface to later damage the articular cartilage. Based upon this data the author’s preferred technique uses the OmniSpan. The control provided by the gun allows for better positioning of the implants and decreased articular cartilage damage. Prototypes of the next generation of OmniSpan (the TrueSpan) perform even better but await clinical experience to confirm our expectations of superior performance.
Complications
All-inside meniscus repair has all the known risks and potential complications of knee arthroscopy. These occur in approximately 1% of patients, and include neurovascular injury, infection, and thrombophlebitis [42]. While neurovascular injuries are likely the most common complication of knee arthroscopy, when compared to other meniscal repair techniques the risk of this complication with all-inside repairs is decreased. Neurologic injury rates as low as 2% have been reported for all-inside techniques, in comparison to 9% for inside-out repairs [43]. The development of the all-inside technique was primarily to eliminate the need for accessory incisions and suture passing that are responsible for most of the neurovascular risk, so that repairs in the posterior horn can be done more safely. Injury to the saphenous nerve is most frequent, but as it is a sensory nerve this is often of little consequence [44]. Peroneal nerve palsy and popliteal artery pseudoaneurysm have also been reported 45, as have cases of cyst formation and synovitis [46, 47]. Complications associated with the adjustable-suture based current generation of all-inside devices include over penetration of the implant, loss of fixation, inadequate tension, and problems with implant deployment [48,49]. An overall complication rate for all-inside repair of 19% has been reported comparable to the gold standard [43]. The RapidLoc has caused cartilage injury in limited reports [50,37], and cadaveric studies have demonstrated placement of these implants may be challenging, but the significance of this is unclear [48,49]. Complications of all-inside repair can be minimized with detailed knowledge of anatomy, proper portal placement, measurement of meniscal depth, and placement of the indicated implant in an appropriate and secure manner.
Rehabilitation:
Post-operative rehabilitation following meniscus repair is highly variable between surgeons, with little consensus in the literature. Early knee motion is thought to be advantageous, as prolonged immobilization is known to lead to stiffness, atrophy, and impaired healing of the meniscus [51]. However, higher degrees of knee flexion cause considerable posterior translation of the femoral condyles, which increases forces within the meniscus and may stress repairs [52]. Weight-bearing can help reduce and stabilize longitudinal (bucket-handle) meniscus tears due to radially directed hoop-stresses [22], but loads with knee flexion cause increasing shear forces in the meniscus. These forces are increased almost four times with the combination of weight-bearing and flexion to 90 degrees [52]. Based on this information, weight-bearing in full extension poses little risk to repairs of longitudinal meniscal tears, and may aid with reduction and healing. However, for radial or meniscal root tear repairs (which are challenging with limited success), weight bearing is not advisable since circumferential fibers are not intact and the tear will be distracted. Accelerated rehabilitation programs designed to return patients to sport earlier have been described [53, 54], permitting early full weight bearing and unrestricted knee motion. The only limitations on return to sport in accelerated programs are the resolution of postoperative effusion, and return of full motion. Thus far, results of accelerated programs have shown return to sport without re-injury or complications. Meniscal repair in the setting of ACL reconstruction presents unique challenges. There is no evidence to support slowing ACL rehabilitation for an associated meniscal repair, and with the increased stability of new adjustable suture-based devices there is less reason to do so 55. The author’s current protocol for modern all-inside devices allows immediate range of motion from 0 to 90 degrees, immediate full weight bearing, early closed-chain strengthening, flexibility and endurance training. After 2 months, full flexion is allowed, and full return sport is permitted once the knee has no effusion, has regained full extension, and demonstrates flexion to greater than 135°.
Conclusions
Advances in arthroscopy and instrumentation technology have made all-inside meniscal repair popular and effective in appropriate meniscal tears. While no arthroscopic method has proven to have superior outcomes in the literature, all-inside methods are indicated for posterior horn meniscal tears to minimize the risk to neurovascular structures. The adjustable suture-based designs have so far demonstrated improved versatility and outcomes comparable to other methods. The versatility of these implants also allows their use in meniscal repairs that are not repairable by other methods, promoting the preservation of meniscal tissue when possible.
References
1. Annandale T. An operation for displaced semilunar cartilage. Br Med J 1885;1:779.
2. Henning CE. Arthroscopic repair of meniscus tears. Orthopedics 1983;6:1130-2.
3. Warren RF. Arthroscopic meniscus repair. Arthroscopy 1985;1:170-2.
4. Ahn JH, Yoo JC, Lee SH. Posterior horn tears: all-inside suture repair. Clin Sports Med;31:113-34.
5. Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res 1980;149:283-90.
6. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med 1986;14:270-5.
7. Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-5.
8. Arnoczky SP, Warren RF. The microvasculature of the meniscus and its response to injury. An experimental study in the dog. Am J Sports Med 1983;11:131-41.
9. Cannon WD, Jr. Arthroscopic meniscal repair. Inside-out technique and results. Am J Knee Surg 1996;9:137-43.
10. Okuda K, Ochi M, Shu N, Uchio Y. Meniscal rasping for repair of meniscal tear in the avascular zone. Arthroscopy 1999;15:281-6.
11. Fitzgibbons RE, Shelbourne KD. “Aggressive” nontreatment of lateral meniscal tears seen during anterior cruciate ligament reconstruction. Am J Sports Med 1995;23:156-9.
12. Zhang Z, Arnold JA, Williams T, McCann B. Repairs by trephination and suturing of longitudinal injuries in the avascular area of the meniscus in goats. Am J Sports Med 1995;23:35-41.
13. Arnoczky SP, Warren RF, Spivak JM. Meniscal repair using an exogenous fibrin clot. An experimental study in dogs. J Bone Joint Surg Am 1988;70:1209-17.
14. Henning CE, Lynch MA, Yearout KM, et al. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res 1990;252:64-72.
15. Sgaglione NA. Meniscus repair update: current concepts and new techniques. Orthopedics 2005;28:280-6.
16. Piontek T, Ciemniewska-Gorzela K, Naczk J, et al. Complex Meniscus Tears Treated with Collagen Matrix Wrapping and Bone Marrow Blood Injection: A 2-Year Clinical Follow-Up. Cartilage 2016;7:123-39.
17. Cannon WD, Jr., Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med 1992;20:176-81.
18. Hanks GA, Gause TM, Handal JA, Kalenak A. Meniscus repair in the anterior cruciate deficient knee. Am J Sports Med 1990;18:606-611.
19. Schmitz MA, Rouse LM, Jr., DeHaven KE. The management of meniscal tears in the ACL-deficient knee. Clin Sports Med 1996;15:573-93.
20. Morrison JB. Function of the knee joint in various activities. Biomed Eng 1969;4:573-80.
21. Richards DP, Barber FA, Herbert MA. Meniscal tear biomechanics: loads across meniscal tears in human cadaveric knees. Orthopedics 2008;31:347-50.
22. Richards DP, Barber FA, Herbert MA. Compressive loads in longitudinal lateral meniscus tears: a biomechanical study in porcine knees. Arthroscopy 2005;21:1452-6.
23. Starke C, Kopf S, Petersen W, Becker R. Meniscal repair. Arthroscopy 2009;25:1033-44.
24. Roeddecker K, Muennich U, Nagelschmidt M. Meniscal healing: a biomechanical study. J Surg Res 1994;56:20-27.
25. Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med 1991;19:632-637.
26. Barber FA, Coons DA. Midterm results of meniscal repair using the BioStinger meniscal repair device. Arthroscopy 2006;22:400-405.
27. Johnson D, Weiss WM. Meniscal repair using the inside-out suture technique. Clin Sports Med 2012;31:15-31.
28. Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect 2000;49:195-206.
29. Morgan CD. The “all-inside” meniscus repair. Arthroscopy 1991;7:120-5.
30. Barrett GR, Treacy SH, Ruff CG. Preliminary results of the T-fix endoscopic meniscus repair technique in an anterior cruciate ligament reconstruction population. Arthroscopy 1997;13:218-23.
31. Borden P, Nyland J, Caborn DN, Pienkowski D. Biomechanical comparison of the FasT-Fix meniscal repair suture system with vertical mattress sutures and meniscus arrows. Am J Sports Med 2003;31:374-8.
32. Barber FA, Herbert MA, Richards DP. Load to failure testing of new meniscal repair devices. Arthroscopy 2004;20:45-50.
33. Quinby JS, Golish SR, Hart JA, Diduch DR. All-inside meniscal repair using a new flexible, tensionable device. Am J Sports Med 2006;34:1281-6.
34. Billante MJ, Diduch DR, Lunardini DJ, et al. Meniscal repair using an all-inside, rapidly absorbing, tensionable device. Arthroscopy 2008;24:779-85.
35. Barber FA, Coons DA, Ruiz-Suarez M. Meniscal repair with the RapidLoc meniscal repair device. Arthroscopy 2006;22:962-6.
36. Hantes ME, Zachos VC, Varitimidis SE, et al. Arthroscopic meniscal repair: a comparative study between three different surgical techniques. Knee Surg Sports Traumatol Arthrosc 2006;14:1232-7.
37. Barber FA. Chondral injury after meniscal repair with rapidLoc. J Knee Surg 2005;18:285-8.
38. Solheim E, Hegna J, Inderhaug E. Long-term outcome after all-inside meniscal repair using the RapidLoc system. Knee Surg Sports Traumatol Arthrosc 2016;24:1495-500.
39. Kalliakmanis A, Zourntos S, Bousgas D, Nikolaou P. Comparison of arthroscopic meniscal repair results using 3 different meniscal repair devices in anterior cruciate ligament reconstruction patients. Arthroscopy 2008;24:810-6.
40. Barber FA, Schroeder FA, Oro FB, Beavis RC. FasT-Fix meniscal repair: mid-term results. Arthroscopy 2008;24:1342-8.
41. Branch EA, Milchteim C, Aspey BS, et al. Biomechanical comparison of arthroscopic repair constructs for radial tears of the meniscus. Am J Sports Med 2015;43:2270-6.
42. Small NC. Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy 1988;4:215-21.
43. Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med 2012;40:459-68.
44. Austin KS. Complications of arthroscopic meniscal repair. Clin Sports Med 1996;15:613-619.
45. Brasseur P, Sukkarieh F. [Iatrogenic pseudo-aneurysm of the popliteal artery. Complication of arthroscopic meniscectomy. Apropos of a case]. J Radiol 1990;71:301-4.
46. Choi NH, Kim SJ. Meniscal cyst formation after inside-out meniscal repair. Arthroscopy 2004;20:E1-3.
47. Kelly JDt, Ebrahimpour P. Chondral injury and synovitis after arthroscopic meniscal repair using an outside-in mulberry knot suture technique. Arthroscopy 2004;20:e49-52.
48. Miller MD, Blessey PB, Chhabra A, Kline AJ, Diduch DR. Meniscal repair with the Rapid Loc device: a cadaveric study. J Knee Surg 2003;16:79-82.
49. Miller MD, Kline AJ, Gonzales J, Beach WR. Pitfalls associated with FasT-Fix meniscal repair. Arthroscopy 2002;18:939-43.
50. Cohen SB, Anderson MW, Miller MD. Chondral injury after arthroscopic meniscal repair using bioabsorbable Mitek Rapidloc meniscal fixation. Arthroscopy 2003;19:E24-6.
51. Dowdy PA, Miniaci A, Arnoczky SP, Fowler PJ, Boughner DR. The effect of cast immobilization on meniscal healing. An experimental study in the dog. Am J Sports Med 1995;23:721-8.
52. Becker R, Wirz D, Wolf C, et al. Measurement of meniscofemoral contact pressure after repair of bucket-handle tears with biodegradable implants. Arch Orthop Trauma Surg 2005;125:254-60.
53. Barber FA. Accelerated rehabilitation for meniscus repairs. Arthroscopy 1994;10:206-10.
54. Mariani PP, Santori N, Adriani E, Mastantuono M. Accelerated rehabilitation after arthroscopic meniscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy 1996;12:680-6.
55. Barber FA, Click SD. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy 1997;13:433-7.
(Abstract) (Full Text HTML) (Download PDF)
Meniscectomy-Outcomes and Complications
Shantanu Sudhakar Patil, Sachin Ramchandra Tapasvi, Anshu Shekhar
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 53-55.
Author: Shantanu Sudhakar Patil[1], Sachin Ramchandra Tapasvi[1], Anshu Shekhar[1].
[1] The Orthopaedic Speciality Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004.
Address of Correspondence
Dr Sachin Ramchandra Tapasvi
The Orthopaedic Speciality Clinic, 16 Status Chambers, 1221/A Wrangler Paranjpe Road, Pune 411004
Email: stapasvi@gmail.com
Abstract
The menisci, once considered expendable remnants have been conclusively proven to be of extreme vitality in the biomechanics and biology of the knee joint. Though meniscus repair is being increasingly performed to preserve knee function, not all tears are amenable to repair and partial meniscectomy in such cases is an acceptable treatment option. The poor outcomes following partial meniscectomy are due to the shrinking of contact areas and rise in peak stresses. These changes and their consequences are more pronounced in the lateral compartment of the knee. Pre-existing chondral damage, instability and higher BMI compound the problem.
Key words: Meniscus, meniscectomy, meniscus repair, arthritis.
Introduction
The menisci of the knee joint are fibrocartilagenous semilunar tissues that perform a critical function of stabilising the joint and aiding in efficient load transfer as a shock absorber. Though once considered vestigial and hence disposable, the role of healthy menisci in delaying the normal attrition of the articular cartilage cannot be understated. Meniscectomy was thought to be a benign procedure and as late as 1975 [1] the importance of doing a complete removal was being reiterated. The functions of the meniscus were recognised much earlier [2] and eventually the potential harms of its excision were gaining attention. Meniscal tears are one of the commonest injuries of the knee, for which treatment is sought, with an incidence rate of 61 per 100000 population per year.[3] Most acute tears are commoner in younger patients, with the medial meniscus affected at a 2:1 ratio with the lateral side. The acute tears are described as per their orientation and extent along the meniscus. They are usually classified as vertical longitudinal, oblique, circumferential, complex, transverse or radial, and horizontal cleavage tears. Radial tears of the posteromedial compartment are the most frequently seen tears and vertical longitudinal tears are most often associated with acute ACL injury. Degenerative tears have a varied pattern and are complex in their morphology.[4]. The direction of the meniscus tears is explained by the orientation of collagen fibrils within the structure. The cross section of the meniscus reveals three distinct layers: a superficial thin layer on both tibial and femoral surfaces; a lamellar layer below this with the fibrils arranged in a radial manner and a main central region where the fibrils are orientated in a circular manner. The circular arrangement of the collagen bundles explains why majority of the tears have a longitudinal orientation. [5](Fig. 1). With our growing understanding of the anatomy , vasculature, biomechanics and the biology of the meniscus, and with improved arthroscopic techniques and instrumentation, the goal of management of meniscal tears has shifted towards achieving repair. However, not all tears are amenable to repair and at least a partial meniscectomy might be indicated to alleviate the patients symptoms. We will take a look at the outcomes and complications of arthroscopic meniscectomy in this article.
Sequelae of articular cartilage changes following Meniscectomy
The effects of meniscectomy on the stability and pressures inside the knee joint were studied using pressure sensitive films in cadavers. Medial meniscectomy caused the contact areas to shrink by almost 75% leading to more than twofold increase in peak contact pressures. [6] The articular cartilage responds unfavourably to the higher loads, with disruption of the proteoglycan matrix, causing swelling and inflammation throughout the joint. The heightened catabolic state with increased hydration leads to breakdown of the collagen matrix, thus accelerating the normal wear and tear within the joint.[7]
Radiological changes:
The radiological changes in the knee joint following medial meniscectomy are well documented.[8]Joint space narrowing, flattening of the marginal part of the medial femoral condyle and sclerosis of the articulating condyles is seen. These radiological signs were indicative of early osteoarthritic changes in the knee. Multiple clinical and radiological studies have documented these sequelae, but the correlation between the symptoms of the patient and severity of these changes is not always seen in the results. It is not easy to determine the correlations as many reports have studied the consequences after an open meniscectomy. Moreover, a meniscal tear rarely presents in isolation and the concomitant ligament or articular injuries play a role in subsequent degeneration and development of Osteoarthritis.
Partial Versus Total meniscectomy
With the advent of arthroscopic surgery and advances in instrumentation for the various surgical procedures, it was possible to resect only the offending parts of the torn meniscus. It is uncommon these days to perform a total resection, with partial meniscectomy being the more widely reported procedure. Once a meniscal tear is identified and deemed unsuitable for repair, a meniscectomy is the recommended surgical option. The basic principles for this were described by Metcalf. They are as follows: Remove all mobile fragments; Avoid sudden changes in rim contour; a perfectly smooth rim is unnecessary as some remodelling may occur; re-evaluate the tear often with a probe; Avoid damage to the meniscus-capsular junction to avoid the loss of hoop stresses; Use both manual and motorized instruments to maximize efficiency and when uncertain if an area should be resected, err on the side of leaving more meniscus intact rather than compromising biomechanical properties[9]. Salata in a meta-analysis showed the significantly higher risk of developing radiographic OA in the patients undergoing total meniscectomy as compared to the partial meniscectomy. [10] Though the patients with either partial or total meniscectomy report similar early clinical results, there was no significant difference in the radiographic outcomes at the final 7.8 years average follow-up[11]. Only 68% of the patients who had undergone a total meniscectomy and followed up for up to 30 years showed good or excellent results while at least 2/3rd had some post-operative symptoms.[12] There exists a direct correlation with the meniscal tissue left behind and peak contact stress on the tibial surfaces following partial resections[13]. A finite element study quantifying the amount of resected meniscus to peak pressures showed that with as little as 20% resection of meniscus, a detrimental increase of forces is seen which may hasten the osteoarthritic changes. Maximum shear stress in the articular cartilage is seen with 65% partial meniscectomy[14]. The orientation of collagen fibril bundles within the meniscus determines the development of hoop strains as they are axially loaded. A radial tear disrupts the continuity of the circularly oriented fibrils and thus prevents the hoop strains from forming, causing dysfunction of the meniscus. A horizontal or vertical tear will not disrupt this continuity, preserving the load-bearing and shock-bearing function of the meniscus.[15] This needs to be borne in mind while determining the extent of the meniscectomy. The medial and lateral tibio-femoral articulations are anatomically different and the absence of menisci which afford a degree of congruity can lead to increased point loading and higher contact pressures. This is more prominent on the lateral side where a convex lateral femoral condyle articulates on a flat or convex tibial plateau. This translates to poorer outcomes with lateral meniscectomy as compared to medial as reported in multiple studies. Patients with a lateral meniscectomy have a much higher functional deterioration and increased instability than the medial meniscectomy patients[11,3,16].
Influence of other concomitant factors
The ACL-deficient knee with a meniscal tear has a significantly higher radiographic grade changes after meniscectomy as compared with ACL-intact knees.[17] Consequences of meniscectomy in an unstable knee are worsened by the combination of higher contact forces inducing early pathological changes due to the elevated shear stresses within the articular cartilage.[18] The presence of pre-existing chondral damage at the time of meniscectomy predisposes the knee to a significant increase in development of OA leading to poor clinical outcomes. However, contradicting findings have also been reported with there being no significant changes in knee functions and activity level following the meniscectomy. [19]. Chondral lesions can cause similar symptoms as that of a meniscal tear and meniscectomy may not fully alleviate the patients’ complaints, thus leading to poor outcomes. Degenerative tears are more often seen in older subjects with varus alignment. However, the evidence that meniscectomy in this group leads to higher rate of radiographic OA is not conclusive. These patients do show a decreased level of activity along with poorer outcomes based on subjective and functional measures following the surgery.[19, 20]While there is consensus about patients with increased BMI predisposing to a higher risk of OA post meniscectomy, the exact level of BMI that placed the patient at risk is not conclusive.[11], [21].
Complications
These can be classified as those related to knee arthroscopy in general and those associated specifically with arthroscopic partial meniscectomy. In the hands of an experienced arthroscopy surgeon, the complication rates were low. (1.78% and 1.48% for medial and lateral meniscectomy) [22], [23]. Some of the enumerated complications include instrument failure or breakage, injuries to nerves and blood vessels, accidental damage to chondral surfaces and ligament injury. Instrument failure rates have dropped from 18.1% to 2.9% over the years, due to improvement in surgical techniques, better designs as well as better skill levels of the surgeons[22]. The medial collateral ligament may get injured due to excessive valgus forces while attempting access to the medial compartment. Similarly, nerves and vessels may get damaged during insertion of sharp instruments. Improper and clumsy handling of instruments during the surgery can gouge the articular surface causing damage. Incomplete removal of the torn pieces can cause persistent pain along with coexistent knee pathology. Proper adherence to basic principles of partial meniscectomy can help avoid all these complications.
Conclusion
There exist a large number of studies which have studied the consequences of meniscectomy as a surgical procedure. Many of these have incomplete or inaccurate information along with varying heterogeneous criteria for evaluation of outcomes. The functional and clinical outcomes do not necessarily match the radiological outcomes in most of the studies. The multiple imaging modalities add to data which is not uniform for evaluation. This lack of homogenous data and lack of standardization of methodological issues, makes it difficult to conclude if the findings represent true differences or are simply artefact related to measurement bias or other errors. It is probably safe to conclude that a minimally invasive procedure with attention to sparing bulk of meniscal tissue seems to reduce the subsequent incidence of arthritic changes, as compared with open invasive and radical procedures..
References
1. Hughston, J.C., A simple meniscectomy. J Sports Med, 1975. 3(4): p. 179-87.
2. King, D., The healing of semilunar cartilages. 1936. Clin Orthop Relat Res, 1990(252): p. 4-7.
3. Jones, J.C., et al., Incidence and risk factors associated with meniscal injuries among active-duty US military service members. J Athl Train, 2012. 47(1): p. 67-73.
4. Pauli, C., et al., Macroscopic and histopathologic analysis of human knee menisci in aging and osteoarthritis. Osteoarthritis Cartilage, 2011. 19(9): p. 1132-41.
5. Petersen, W. and B. Tillmann, Collagenous fibril texture of the human knee joint menisci. Anat Embryol (Berl), 1998. 197(4): p. 317-24.
6. Baratz, M.E., F.H. Fu, and R. Mengato, Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med, 1986. 14(4): p. 270-5.
7. Lanzer, W.L. and G. Komenda, Changes in articular cartilage after meniscectomy. Clin Orthop Relat Res, 1990(252): p. 41-8.
8. Fairbank, T.J., Knee joint changes after meniscectomy. J Bone Joint Surg Br, 1948. 30b(4): p. 664-70.
9. Metcalf, R.W., Arthroscopic meniscal surgery., in Operative Arthroscopy., M. JB, Editor. 1991, Raven Press: New York. p. pp. 203–236.
10. Salata, M.J., A.E. Gibbs, and J.K. Sekiya, A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med, 2010. 38(9): p. 1907-16.
11. Hede, A., E. Larsen, and H. Sandberg, Partial versus total meniscectomy. A prospective, randomised study with long-term follow-up. J Bone Joint Surg Br, 1992. 74(1): p. 118-21.
12. Tapper, E.M. and N.W. Hoover, Late results after meniscectomy. J Bone Joint Surg Am, 1969. 51(3): p. 517-26 passim.
13. Ihn, J.C., S.J. Kim, and I.H. Park, In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop, 1993. 17(4): p. 214-8.
14. Vadher, S.P., et al., Finite element modeling following partial meniscectomy: effect of various size of resection. Conf Proc IEEE Eng Med Biol Soc, 2006. 1: p. 2098-101.
15. Jones, R.S., et al., Direct measurement of hoop strains in the intact and torn human medial meniscus. Clin Biomech (Bristol, Avon), 1996. 11(5): p. 295-300.
16. Petty, C.A. and J.H. Lubowitz, Does arthroscopic partial meniscectomy always cause arthritis? Sports Med Arthrosc, 2012. 20(2): p. 58-61.
17. Burks, R.T., M.H. Metcalf, and R.W. Metcalf, Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy, 1997. 13(6): p. 673-9.
18. McDermott, I.D. and A.A. Amis, The consequences of meniscectomy. J Bone Joint Surg Br, 2006. 88(12): p. 1549-56.
19. Rockborn, P. and J. Gillquist, Long-term results after arthroscopic meniscectomy. The role of preexisting cartilage fibrillation in a 13 year follow-up of 60 patients. Int J Sports Med, 1996. 17(8): p. 608-13.
20. Chatain, F., et al., The natural history of the knee following arthroscopic medial meniscectomy. Knee Surgery, Sports Traumatology, Arthroscopy, 2000. 9(1): p. 15-18.
21. Englund, M. and L.S. Lohmander, Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum, 2004. 50(9): p. 2811-9.
22. Small, N.C., Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy, 1988. 4(3): p. 215-21.
23. Allum, R., Complications of arthroscopy of the knee. J Bone Joint Surg Br, 2002. 84(7): p. 937-45.
24. Papalia, R., et al., Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull, 2011. 99: p. 89-106.
(Abstract) (Full Text HTML) (Download PDF)
Menisci: Structure and Function
Ankit Chawla, Amite Pankaj Aggarwal
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 3-7
Author: Ankit Chawla[1], Amite Pankaj Aggarwal[1]
[1] Unit of Joint Replacement, Arthroscopy and Orthopaedics, Fortis Hospital, Shalimar Bagh, New Delhi, India.
Address of Correspondence
Dr. Amite Pankaj Aggarwal
Fortis Hospital Shalimar Bagh
New Delhi, India.
Email: amitepankaj@gmail.com.
Abstract
Meniscal injuries are recognized as a cause of significant musculoskeletal morbidity. The menisci are vital for the normal function and long-term health of the knee joint. And loss of a meniscus increases the risk of subsequent development of degenerative changes in the knee. A review of anatomy and ultrastructure of the meniscus, and its relationship to normal function in terms of load transmission, shock absorption, joint stability, lubrication and nutrition is a necessary prerequisite to understanding pathologies associated with the knee.
Keywords: Meniscus, Medial meniscus, lateral meniscus, Anatomy, Function.
Introduction
The word meniscus comes from the Greek word me-niskos, meaning “crescent,” diminutive of me-ne-, meaning “moon.” The menisci are semilunar discs of fibrocartilaginous tissue which are vital for the normal biomechanics and long-term health of the knee joint [1]. The characteristic shape of the lateral and medial menisci is attained between the 8th and 10th week of gestation. They arise from a condensation of the intermediate layer of mesenchymal tissue to form attachments to the surrounding joint capsule[2,3].
Gross Anatomy
These crescent-shaped wedges of fibrocartilage are located on the medial and lateral aspects of the knee joint (Fig. 1A,1B). The peripheral, vascular border of each meniscus is thick, convex, and attached to the joint capsule. The innermost border tapers to a thin free edge. The superior surfaces of menisci are concave, enabling effective articulation with their respective convex femoral condyles. The inferior surfaces are flat to accommodate the tibial plateau [4,5].
Medial Meniscus
The medial meniscus is a C-shaped structure larger in radius than the lateral meniscus, with the posterior horn being wider than the anterior. The anterior horn is attached firmly to the tibia anterior to the intercondylar eminence and to the anterior cruciate ligament. The posterior horn is anchored immediately in front of the attachments of the posterior cruciate ligament posterior to the intercondylar eminence. Its entire peripheral border is firmly attached to the medial capsule and through the coronary ligament to the upper border of the tibia. At its midpoint, the medial meniscus is more firmly attached to the femur through a condensation in the joint capsule known as the deep medial collateral ligament [5]. The transverse, or “intermeniscal,” ligament is a fibrous band of tissue that connects the anterior horn of the medial meniscus to the anterior horn of the lateral meniscus [5,6].
Lateral Meniscus
The lateral meniscus is more circular in form, covering up to two thirds of the articular surface of the underlying tibial plateau [7]. The anterior horn is attached to the tibia medially in front of the intercondylar eminence, whereas the posterior horn inserts into the posterior aspect of the intercondylar eminence and in front of the posterior attachment of the medial meniscus. The lateral meniscus is loosely attached to the capsular ligament; however, these fibers do not attach to the lateral collateral ligament. The posterior horn of the lateral meniscus attaches to the inner aspect of the medial femoral condyle via the anterior and posterior meniscofemoral ligaments of Humphrey and Wrisberg, respectively, which originate near the origin of the PCL (Fig. 1A) [8]. Their estimated prevalence is 74 % for Humphrey ligament, 69 % for Wrisberg ligament, and both ligaments found together in around 50 % of knees [9]. The lateral meniscus is smaller in diameter, thicker in periphery, wider in body, and more mobile than the medial meniscus.
Extracellular matrix and cellularity
Considering composition by wet weight, the meniscus has high water content (72 %). The remaining 28 % consists of an organic component, mostly ECM and cells.10 Collagens comprise the majority (75 %) of the organic matter, followed by GAGs (17 %), DNA (2 %), adhesion glycoproteins (<1 %), and elastin (<1 %) [10,11]. These proportions vary according to age, injury, or pathological conditions [12]. Collagen is the main fibrillar component of the meniscus. Different collagen types exist in various quantities in each region of meniscus. In the red–red zone, type I collagen is predominant (80 % composition in dry weight). In the white–white zone, 60 % is type II collagen and 40 % is type I collagen [13]. The major orientation of collagen fibers in the meniscus is circumferential; radial fibers and perforating fibers also are present.(Fig. 3) [13]. Proteoglycans are heavily glycosylated molecules that constitute a major component of the meniscus ECM [14]. These molecules are comprised of a core protein which is decorated with glycosaminoglycans (GAGs). The main types of GAGs found in normal human meniscal tissue are chondroitin 6 sulfate (60%), dermatan sulfate(20-30%), chondroitin 4 sulfate (10-20%), and keratin sulfate(15%) [15]. Their main function is to enable the meniscus to absorb water, whose confinement supports the tissue under compression [10]. Adhesion glycoproteins are also important components of the meniscus matrix, as they serve as a link between ECM components and cells [16]. The main adhesion glycoproteins present in the human meniscus are fibronectin, thrombospondin, and collagen VI [16,17]. Outer zone cells have an oval, fusiform shape and are similar in appearance and behaviour to fibroblasts, described as fibroblast-like cells [18]. The matrix surrounding the cells is mainly comprised of type I collagen, with small percentages of glycoproteins and collagen types III and V present. In contrast, cells in the inner portion have rounded appearance and are embedded in an ECM comprising largely type II collagen intermingled with a smaller but significant amount of type I collagen and higher concentration of GAGs [18]. This relative abundance of collagen type II and aggrecan in the inner region is more reminiscent of hyaline articular cartilage. Therefore, cells in this region are classified as fibrochondrocytes or chondrocyte like cells. In summary, cell phenotype and ECM composition render the outer portion of the meniscus akin to fibrocartilage, while the inner portion possesses similar, but not identical, traits to articular cartilage [19,20].
Vascularity and Innervation
The vascular supply to the medial and lateral menisci originates predominantly from the lateral and medial geniculate vessels (both inferior and superior). Branches from these vessels give rise to a perimeniscal capillary plexus within the synovial and capsular tissue. (Fig. 2) Radial branches from the plexus enter the meniscus at intervals, with a richer supply to the anterior and posterior horns. Vessels supplying the body are limited to the meniscus periphery with a variable penetration of 10–30 % for medial meniscus and 10–25 % for lateral one. This has important implication for meniscal healing [21]. The remaining portion of each meniscus (65% to 75%) receives nourishment from synovial fluid via diffusion or mechanical pumping (ie, joint motion) [22, 23]. The knee joint is innervated by the posterior articular branch of the posterior tibial nerve and the terminal branches of the obturator and femoral nerves. The lateral portion of the capsule is innervated by the recurrent peroneal branch of the common peroneal nerve. These nerve fibers penetrate the capsule and follow the vascular supply to the peripheral portion of the menisci and the anterior and posterior horns, where most of the nerve fibers are concentrated. The inner menisci core has no nerve fibers [21].
Biomechanical Function
The biomechanical function of the meniscus is a reflection of the gross and ultrastructural anatomy and of its relationship to the surrounding intra-articular and extra-articular structures. The meniscus withstands many different forces such as shear, tension, and compression. It also plays a crucial role in load-bearing, load transmission, shock absorption, stability, propioception as well as lubrication and nutrition of articular cartilage [24-27]. They also serve to decrease contact stresses and increase contact area and congruity of the knee [28,29].
Meniscal Biomechanics
The biomechanical properties of the knee meniscus are appropriately tuned to withstand the forces exerted on the tissue. Many studies have helped to quantify the properties of the tissue both in humans and in animal models. According to these studies, the meniscus resists axial compression with an aggregate modulus of 100-150 kPa [30]. The tensile modulus of the tissue varies between the circumferential and radial directions; it is approximately 100-300 MPa circumferentially and 10 fold lower than this radially [31]. Finally, the shear modulus of the meniscus is approximately 120 kPa [31]. The contact forces on the meniscus within the human knee joint have been mapped. It has been calculated that the intact menisci occupy approximately 60% of the contact area between the articular cartilage of the femoral condyles and the tibial plateau, while they transmit >50% of the total axial load applied in the joint [32,33]. However, these percentages are highly dependent on degree of knee flexion and tissue health. For every 30o of knee flexion, the contact surface between the two knee bones decreases by 4% [34]. When the knee is in 90o of flexion the applied axial load in the joint is 85% greater than when it is in 0o of flexion [33]. In full knee flexion, the lateral meniscus transmits 100% of the load in the lateral knee compartment, whereas the medial meniscus takes on approximately 50% of the medial load [29]. Studies confirm that there is a significant difference in segmental motion during flexion between the medial and lateral menisci. The anterior and posterior horn lateral meniscus ratio is smaller and indicates that the meniscus moves more as a single unit [35]. Alternatively, the medial meniscus (as a whole) moves less than the lateral meniscus, displaying a greater anterior to posterior horn differential excursion. Thompson et al found that the area of least meniscal motion is the posterior medial corner, where the meniscus is constrained by its attachment to the tibial plateau by the meniscotibial portion of the posterior oblique ligament, which has been reported to be more prone to injury [35,36]. A reduction in the motion of the posterior horn of the medial meniscus is a potential mechanism for meniscal tears, with a resultant “trapping” of the fibrocartilage between the femoral condyle and the tibial plateau during full flexion. The greater differential between anterior and posterior horn excursion may place the medial meniscus at a greater risk of injury [35]. The differential of anterior horn to posterior horn motion allows the menisci to assume a decreasing radius with flexion, which correlates to the decreased radius of curvature of the posterior femoral condyles [35]. This change of radius allows the meniscus to maintain contact with the articulating surface of both the femur and the tibia throughout flexion.
Load Transmission
Fairbank described the increased incidence and predictable degenerative changes of the articular surfaces in completely meniscectomized knees [37]. Weightbearing produces axial forces across the knee, which compress the menisci, resulting in “hoop” (circumferential) stresses [38]. Hoop stresses are generated as axial forces and converted to tensile stresses along the circumferential collagen fibers of the meniscus. Firm attachments by the anterior and posterior insertional ligaments prevent the meniscus from extruding peripherally during load bearing [39]. Medial meniscectomy decreases contact area by 50% to 70% and increases contact stress by 100%. Lateral meniscectomy decreases contact area by 40% to 50% but dramatically increases contact stress by 200% to 300% because of the relative convex surface of the lateral tibial plateau [40,41]. This significantly increases the load per unit area and may contribute to accelerated articular cartilage damage and degeneration [42].
Shock absorption
The menisci play a vital role in attenuating the intermittent shock waves generated by impulse loading of the knee with normal gait [43,44]. Voloshin and Wosk showed that the normal knee has a shock-absorbing capacity about 20% higher than knees that have undergone meniscectomy [38]. As the inability of a joint system to absorb shock has been implicated in the development of osteoarthritis, the meniscus would appear to play an important role in maintaining the health of the knee joint [45]
Joint stability
The geometric structure of the menisci provides an important role in maintaining joint congruity and stability. The superior surface of each meniscus is concave, enabling effective articulation between the convex femoral condyles and flat tibial plateau. When the meniscus is intact, axial loading of the knee has a multidirectional stabilizing function, limiting excess motion in all directions [46]. The studies for effects of meniscectomy on joint laxity for anteroposterior and varus-valgus motions and rotation have indicated indicated that the effect on joint laxity depends on whether the ligaments of the knee are intact and whether the joint is bearing weight. In the presence of intact ligamentous structures, excision of the menisci produces small increases in joint laxity. In an anterior cruciate ligament–deficient knee, medial meniscectomy has been shown to increase tibial translation by 58% at 90o, whereas primary anterior and posterior translations were not affected by lateral meniscectomy [47]. Shoemaker and Markolf demonstrated that the posterior horn of the medial meniscus is the most important structure resisting an anterior tibial force in the ACL-deficient knee. [48] Recently, Musahl et al reported that the lateral meniscus plays a role in anterior tibial translation during the pivot-shift maneuver [49].
Joint Nutrition and Lubrication
The menisci may also play a role in the nutrition and lubrication of the knee joint. The mechanics of this lubrication remains unknown; the menisci may compress synovial fluid into the articular cartilage, which reduces frictional forces during weightbearing [50]. There is a system of microcanals within the meniscus located close to the blood vessels, which communicates with the synovial cavity; these may provide fluid transport for nutrition and joint lubrication [51,52].
Conclusions
Mechanoreceptors have been identified in the anterior and posterior horns of the menisci, middle and outer third of the meniscus. The identification of these neural elements indicates that the menisci are capable of detecting proprioceptive information (joint motion and position) in the knee joint, thus playing an important afferent role in the sensory feedback mechanism of the knee [53,54].
References
1. McDermott ID, Masouros SD, Amis AA. Biomechanics of the menisci of the knee. Curr Orthopaed.2008 ;22:193–201
2. Gardner E, O’Rahilly R. The early development of the knee joint in staged human embryos. J Anat.1968;102:289-299.
3. Gray DJ, Gardner E. Pre-natal development of the human knee and superior tibial fibula joints. Am J Anat.1950;86:235-288.
4. Bullough PG, Vosburgh F, Arnoczky SP, et al. The menisci of the knee. In: Insall JN, ed. Surgery of the Knee. New York, NY: Churchill Livingstone; 1984:135-149.
5. Warren RF, Arnoczky SP, Wickiewiez TL. Anatomy of the knee. In: Nicholas JA, Hershman EB, eds. The Lower Extremity and Spine in Sports Medicine. St. Louis: Mosby; 1986:657-694.
6. Johnson DL, Swenson TD, Harner CD. Arthroscopic meniscal transplantation: anatomic and technical considerations. Presented at: Nineteenth Annual Meeting of the American Orthopaedic Society for Sports Medicine; July 12-14, 1993; Sun Valley, ID.
7. Arnoczky SP, Adams ME, DeHaven KE, Eyre DR, Mow VC. The meniscus. In: Woo SL-Y, Buckwalter J, eds. Injury and Repair of Musculoskeletal Soft Tissues. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1987:487-537.
8. Johnson DL, Swenson TM, Livesay GA, Aizawa H, Fu FH, Harner CD. Insertion-site anatomy of the human menisci: gross, arthroscopic, and topographical anatomy as a basis for meniscal transplantation. Arthroscopy.1995;11:386-394.
9. Heller L, Langman J. The meniscofemoral ligaments of the human knee. J Bone Joing Surg Br.1964;46 :307-313.
10. Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011 Oct;32(30):7411-31.
11. Herwig J, Egner E, Buddecke E. Chemical changes of human knee joint menisci in various stages of degeneration. Ann Rheum Dis. 1984 Aug;43(4):635-40.
12. Sweigart MA, Athanasiou KA. Toward tissue engineering of the knee meniscus. Tissue Eng. 2001 Apr;7(2):111-29.
13. Cheung HS. Distribution of type I, II, III and V in the pepsin solubilized collagens in bovine menisci. Connect Tissue Res. 1987;16(4):343-56.
14. Beaupre A, Choukroun R, Guidouin R, Carneau R, Gerardin H. Knee menisci: correlation between microstructure and biomechanics. Clin Orthop Relat Res.1986 ;208 :72-75.
15. Assimakopoulos AP, Katonis PG, Agapitos MV, Exarchou EI. The innervations of the human meniscus. Clin Orthop Relat Res.1992;275:232-236.
16. Miller RR, McDevitt CA. Thrombospondin in ligament, meniscus and intervertebral disc. Biochim Biophys Acta. 1991 Nov 14;1115(1):85-8
17. McDevitt CA, Webber RJ. The ultrastructure and biochemistry of meniscal cartilage. Clin Orthop Relat Res. 1992; 252:8–18.
18. Verdonk PC, Forsyth RG, Wang J et al (2005) Characterisation of human knee meniscus cell phenotype. Osteoarthritis Cartilage 13:548–560.
19. Melrose J, Smith S, Cake M, Read R, Whitelock J. Comparative spatial and temporal localisation of perlecan, aggrecan and type I, II and IV collagen in the ovine meniscus: an ageing study. Histochem Cell Biol. 2005; 124:225–35.
20. Hellio Le Graverand MP, Ou Y, Schield-Yee T, Barclay L, Hart D, Natsume T, et al. The cells of the rabbit meniscus: their arrangement, interrelationship, morphological variations and cytoarchitecture. J Anat. 2001; 198:525–35.
21. Brian D, Mackenzie WG, Shim SS, Leung G (1985) The vascular and nerve supply of the human meniscus. Arthroscopy 1:58–62.
22. Meyers E, Zhu W, Mow V. Viscoelastic properties of articular cartilage and meniscus. In: Nimni M, ed. Collagen: Chemistry, Biology and Biotechnology. Boca Raton, FL: CRC; 1988.
23. Mow V, Fithian D, Kelly M. Fundamentals of articular cartilage and meniscus biomechanics. In: Ewing JW, ed. Articular Cartilage and Knee Joint Function: Basic Science and Arthroscopy New York, NY: Raven Press; 1989:1-18.
24. Cameron HU, Macnab I. The structure of the meniscus of the human knee joint. Clin Orthop Relat Res. 1972; 89:215–9.
25. Newman AP, Anderson DR, Daniels AU, Dales MC. Mechanics of the healed meniscus in a canine model. Am J Sports Med. 1989; 17:164–75.
26. Zhu W, Chern KY, Mow VC. Anisotropic viscoelastic shear properties of bovine meniscus. Clin Orthop Relat Res. 1994; 306:34–45.
27. Tissakht M, Ahmed AM, Chan KC. Calculated stress-shielding in the distal femur after total knee replacement corresponds to the reported location of bone loss. J Orthop Res. 1996; 14:778–85.
28. Kettelkamp DB, Jacobs AW. Tibiofemoral contact area: determination and implications. J Bone Joint Surg Am. 1972;54:349-356.
29. Walker PS, Erkman MJ. The role of the meniscus in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184-192.
30. Sweigart MA, Zhu CF, Burt DM, DeHoll PD, Agrawal CM, Clanton TO, et al. Intraspecies and interspecies comparison of the compressive properties of the medial meniscus. Ann Biomed Eng. 2004; 32:1569–79.
31. Fithian DC, Kelly MA, Mow VC. Material properties and structure-function relationships in the menisci. Clin Orthop Relat Res. 1990; 252:19–31.
32. Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980; 51:871–9.
33. Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints—Part I: Tibial surface of the knee. J Biomech Eng. 1983; 105:216–25.
34. Walker PS, Hajek JV. The load-bearing area in the knee joint. J Biomech. 1972; 5:581–9.
35. Thompson WO, Thaete FL, Fu FH, Dye SF. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance imaging. Am J Sports Med.1991;19:210-216.
36. Ricklin P, Ruttimann A, Del Bouno MS. Diagnosis, Differential Diagnosis and Therapy. 2nd ed. Stuttgart, Germany: Verlag Georg Thieme; 1983
37. Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br.1948;30:664-670.
38. Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomed Eng.1983 ;5 :157-161.
39. Krause WR, Pope MH, Johnson RJ, Wilder DG. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976;58:599-604.
40. Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee: a study of normal and osteoarthritic knee joints. Acta Orthop Scand.1980;51:871-879.
41. Kettelkamp DB, Jacobs AW. Tibiofemoral contact area: determination and implications. J Bone Joint Surg Am.1972;54:349-356.
42. Jones RE, Smith EC, Reisch JS. Effects of medial meniscectomy in patients older than forty years. J Bone Joint Surg Am.1978;60:783-786.
43. Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res.1980;149:283-290.
44. Seedhom BB, Hargreaves DJ. Transmission of the load in the knee joint with special reference to the role in the menisci: part II. Experimental results, discussion and conclusion. Eng Med.1979;8:220-228.
45. Radin EL, Rose RM. Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop Relat Res.1986 ;213:34-40.
46. Arnoczky SP. Gross and vascular anatomy of the meniscus and its role in meniscal healing, regeneration and remodeling. In: Mow VC, Arnoczky SP, Jackson SW, eds. Knee Meniscus: Basic and Clinical Foundations New York, NY: Raven Press; 1992:1-14.
47. Markolf KL, Mensch JS, Amstutz HC. Stiffness and laxity of the knee: the contributions of the supporting structures. J Bone Joint Surg Am.1976;58:583-597.
48. Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee: effects of partial versus total excision. J Bone Joint Surg Am.1986 ; 68 (1):71-79.
49. Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010 ;38 (8) :1591-1597.
50. Arnoczky SP, Warren RF, Spivak JM. Meniscal repair using exogenous fibrin clot: an experimental study in dogs. J Bone Joint Surg Am.1988;70:1209-1217.
51. Bird MDT, Sweet MBE. Canals of the semilunar meniscus: brief report. J Bone Joint Surg Br.1988 ;70 : 839.
52. Bird MDT, Sweet MBE. A system of canals in semilunar menisci. Ann Rheum Dis.1987;46 : 670 – 673.
53. Karahan M, Kocaoglu B, Cabukoglu C, Akgun U, Nuran R. Effect of partial medial meniscectomy on the proprioceptive function of the knee. Arch Orthop Trauma Surg.2010;130:427-431.
54. Skinner HB, Barrack RL, Cook SD. Age-related decline in proprioception. Clin Orthop Relat Res.1984;184:208-211..
(Abstract) (Full Text HTML) (Download PDF)
Meniscal Scaffolds in the Clinics: Present and Future Trends
Ricardo Bastos, Renato Andrade, Hélder Pereira, J Miguel Oliveira, Rui L Reis, Scott Rodeo, João Espregueira-Mendes.
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 47-52.
Author: Ricardo Bastos[1,2,3], Renato Andrade[2,3,4], Hélder Pereira[5,6,7,8], J Miguel Oliveira, Rui L Reis, Scott Rodeo, João Espregueira-Mendes[2,3,5,6,14].
[1] Universidade Federal Fluminense, Nireói, Rio de Janeiro, Brazil.
[2] Clínica do Dragão, Espregueira-Mendes Sports Centre – FIFA Medical Centre of Excellence, Porto, Portugal.
[3] Dom Henrique Research Centre, Porto, Portugal.
[4] Faculty of Sports, University of Porto, Porto, Portugal.
[5] 3B’s Research Group – Biomaterials, Biodegradables and Biomimetics, University of Minho, Headquarters of the European Institute of Excellence on Tissue Engineering and Regenerative Medicine, AvePark- Parque de Ciência e Tecnologia, 4805-017 Barco, Guimarães, Portugal.
[6] – ICVS/3B’s – PT Government Associated Laboratory, Braga/Guimarães, Portugal.
[7] – Orthopaedic Department, Centro Hospitalar Póvoa de Varzim – Vila do Conde, Póvoa de Varzim, Portugal.
[8] – Ripoll y De Prado Sports Clinic FIFA Medical Centre of Excellence, Murcia-Madrid, Spain.
[9] – Co-Chief Emeritus, Sports Medicine and Shoulder Service, Hospital for Special Surgery, New York, USA.
[10] – Co-Director, Tissue Engineering, Regeneration, and Repair Program, New York, USA.
[11] – Orthopaedic Surgery, Weill Medical College of Cornell University, New York, USA.
[12] – Attending Orthopaedic Surgeon, Hospital for Special Surgery, New York, USA.
[13] – Head Team Physician, New York Giants Football, New York, USA.
[14] – Orthopaedics Department of Minho University, Minho, Portugal.
Address of Correspondence
Dr. João Espregueira-Mendes; Via Futebol Clube do Porto – F. C. Porto Stadium, Porto, Portugal; +351 220 100 100; Email: espregueira@dhresearchcentre.com
Abstract
Despite the high incidence, meniscal lesions still remain a clinical challenge due to its limited regenerative ability. In the last two decades, the development of scaffolding strategies has revolutionized meniscus treatment possibilities. Along with these new developments, the orthopaedic community has embraced the campaign “preserve the meniscus”. In this sense, acellular or cellularized scaffolds have emerged as a potential solution to treat irreparable meniscal lesions. Herein, it are overviewed the up-to-date acellular meniscal scaffolds used in the clinics, indications and discussed their outcomes.
Keywords: Meniscal scaffolds; Meniscal implants; Meniscal substitutes.
Introduction
The menisci have been described as a two-edge shaped semilunar discs of fibrocartilaginous tissue, found at the medial and lateral compartment of the tibiofemoral joint (1, 2). They play a fundamental role in many aspects of knee function, including articular congruency and stability, load distribution, shock absorption as well as a role in joint lubrication and proprioception (3). Many of these functions are achieved through the ability to transmit and distribute load over t The medial anhe tibial plateaus.d lateral menisci can transmit from 50% up to 70% of the load when the knee is in extension, and up to 85% at 90 degrees of knee flexion (4). Removal of the medial meniscus can result in a 50% to 70% reduction in femoral condyle cartilage contact area and a 100% increase in contact stress (5). Total lateral meniscectomy causes a 40% to 50% decrease in cartilage contact area and increases contact stress in the lateral compartment up to 200% to 300% of normal. Furthermore, even just partial removal of the meniscus does alter joint loading, particularly when two thirds of the posterior horn is excised (6). Despite the importance of the meniscus structure and the need for its preservation, meniscal lesions are the most common surgically treated knee pathology, and their annual incidence can be estimated at 60-70 per 100,000 knees, with 850,000 meniscal procedures performed yearly only in the United States (7) and 400,000 in Europe (8). For several years, the meniscus function was not fully understood. Recent pre-clinical and clinical evidences support the idea that the preservation of the meniscus structure is of outmost importance (9, 10). Thus, tissue engineering approaches have gain great attention as promise to regenerate different tissues and organs, including meniscus tissue (11-15). It has provided a fundamental understanding and technology that have permitted the development of scaffolds derived from biological tissues and synthetic materials, and there is currently a large amount of active, ongoing research into meniscus scaffolds (16-18). The meniscus scaffolds have been mainly limited to the treatment of meniscus partial repair once it requires an undamaged meniscal rim and enough tissue at the anterior and posterior horns to allow the fixation of the scaffold to the remaining meniscal tissues.
Types of Scaffolds
Scaffold biomechanical structure must have adequate material properties to allow tissue regeneration, while protecting the newly-forming tissue from excessive stresses. Their absorption must be sufficiently gradual, allowing appropriate cell migration, formation of new vessels, and matrix synthesis in order to create meniscal-like tissue (19, 20). At the same time, the scaffold and its degradation products should not damage the articular surface or invoke a foreign body reaction. An important step in the preparation of acellular meniscal scaffolds is the ability of mimicking the architectural and geometric complexity of the native tissue (20, 21). In this sense, it is crucial to further understand the menisci anatomy, biology, ultrastructure and biomechanical function to enhance the success of the meniscal substitution (1, 13). Two scaffolds are currently in clinical use.
Collagen Meniscus Implant (CMI, Ivy Sports Medicine GmbH, Germany) – First published in 1997, CMI is a type-I collagen (isolated and purified from bovine Achilles tendon) scaffold (22) to which glycosaminoglycans are added. It has a meniscus-like shape, is implantable arthroscopically, and it is biocompatible and biodegradable. It has a microscopic porous structure that allows cellular ingrowth, induces differentiation and proliferation of fibrocartilaginous cells, leading to the creation of a meniscus-like tissue, concomitant with gradual resorption of the scaffold. Nevertheless, collagen scaffolds are fragile during the implant procedure, and have shown a decrease in size on follow-up magnetic resonance image (MRI) and arthroscopic second look follow-up. The second type of scaffold is Actifit® (Orteq, United Kingdom) that has been developed to overcome the perceived limitations of CMI related to difficulties in tissue handling with respect to suturing during implantation (Figure 1). Actifit® is composed of a slowly degrading polymer with polycaprolactone and urethane segments (23). Its structure seems to have better mechanical properties and is more resistant to sutures and loads as compared to CMI. The scaffold is 80% porous; the remaining 20% are made of a polymer with a low absorption rate. Degradation starts with hydrolysis of polycaprolactone segments, which lasts up to five years; the polyurethane segments are removed by macrophages and giants cells or integrated into surrounding tissues (24, 25).
Indications – Contraindications
When considering meniscal scaffolding, the surgeon should take into account several individual aspects, such as the patient’s age and weight, status of meniscal degeneration or concomitant conditions (such as axial malalignment and ligamentous insufficiency) (26). In this sense, several indications and contraindications have been developed as summarized in Table 1.
Preoperative Preparation
The preoperative imaging preparation usually involves radiography, MRI and, in some special cases, an arthro-computed tomography (arthro-CT). The radiographic imaging studies usually include bilateral comparison of weight-bearing radiographs (antero-posterior, lateral, Schuss or Rosenberg views). The MRI is usually performed to assess the cartilaginous structures status, quantify the meniscal damage, as well as the presence of bone marrow edema and/or meniscal extrusion (Figure 2). The arthro-CT scan may complement the MRI studies by assessing the meniscal volume and chondral damage (26). The imaging studies should be complemented with a comprehensive clinical examination of the knee. Special attention should be given to the knee ligament stability, as this has several implications in the meniscal surgery. In addition, diagnostic arthroscopy (Figure 3) may be performed to further assess the meniscal status and decide upon the best technique (26).
Surgical Technique
The procedure can be performed arthroscopically using the two standard anteromedial and anterolateral portals. The portals should be enlarged for an easier passage of the scaffold. The native remaining meniscus is thoroughly evaluated, and any torn or degenerative tissue is removed in order to leave a healthy and uniform meniscal rim, ensuring that the resulting defect site extends into the vascularized red-on-red or red-on-white zone of the meniscus. The meniscal rim is punctured in order to create vascular access channels. Gentle rasping of the synovial lining may further stimulate meniscal integration and tissue ingrowth. The exact size of the defect is measure with a flexible rod loaded in a rigid cannula starting at the posterior end of the lesion. The scaffold is measured and trimmed to the correct size on the sterile field of the operating environment (10% larger than in situ measurement to compensate for the shrinkage caused by suturing of the sponge-like material and to assure a snug optimal fit into the prepared defect). In order to achieve a perfect fit of the scaffold with the native meniscus at the anterior junction, the anterior side should be cut at an oblique angle of 30°-45°. The implant is inserted into the defect (Figure 4). Standard arthroscopic meniscal suturing techniques may be utilized for scaffold stabilization. The authors prefer “all-inside” vertical stitches placed every 4 to 5 mm to suture the scaffold along the periphery. The anterior and posterior scaffold extremities are fixed to the native remnant with horizontal stitches.
Concomitant Surgeries
Since other associated deficiencies (such as axial malalignment or ligamentous instability) may lead to poorer outcomes following meniscal surgery, these should be address in combination with the meniscal substitution (27). Anterior cruciate ligament insufficiency, if not addressed, may result in residual laxity, which may lead to an unfavorable meniscal healing environment. In this sense, ACL reconstruction has been performed along with the meniscal substitution in up to 67% of the patients (28-30). When performing concomitant ACL reconstruction, the meniscal bed should be firstly prepared and then the tibial and femoral tunnels may be drilled. After the tunnels are drilled, the ACL graft is passed through the tunnels and fixed at the femoral site, as the meniscal scaffold is inserted and sutured. Subsequently, the ACL graft is fixed at the tibial site with 20° of knee flexion (31). When uncorrected axial knee malalignments are found, these should be concomitantly or previously corrected. In a varus malalignment situation, a high tibial osteotomy may be performed to correct the malalignment. Special attention must be directed to the tibial slope and proper release of the medial collateral ligament should be performed. In valgus malalignments, if the deformity does not involve the tibial bone, osteotomy is done on the femoral side to avoid joint line obliquity (27).
Rehabilitation protocol
Patients are required to undergo a conservative rehabilitation program similar to that for a meniscal allograft. Special attention is required when the meniscal scaffold is implanted with concomitant ACL reconstruction or realignment osteotomy. In these cases, a rehabilitation program should be tailored to comply with the concomitant procedures postoperative particularities (26, 27). General guidelines for the rehabilitation program are presented in Table 3.
Clinical Studies
Although the literature contains clinical studies (33-35) that support the use of meniscal scaffold implantation for the treatment of irreparable meniscal tears, the quality of the studies is generally low, with lack of randomized trials and long-term follow-up to confirm clinical benefit and the most appropriate indications. Furthermore, long-term follow-up studies are required to verify the protective effect on the damaged joint compartment exerted by meniscal scaffold implantation.
A recent systematic literature review (35) analyzed results and indications for the treatment of meniscal loss. There has been an increase in publications regarding this topic recently, and the authors concluded that both CMI and Actifit seem to be safe and positive results have been shown for both scaffolds. Bulgheroni et al. (36) evaluated the safety and effectiveness of the polyurethane meniscal scaffold through clinical examination, MRI and arthroscopic second look, over a minimum two-year follow-up and showed no adverse reactions to the implant. The implant showed clear, hyperintense signal, sometimes irregular, and the chondral surface was preserved in all cases. At arthroscopic second look at 12 and 24 months, the scaffold was found to have an irregular morphology and to be slightly reduced in size. Zafagnini et al. (37), in a 10-year follow-up study, compared the medial collagen meniscus implant versus partial medial meniscectomy. The CMI group showed significantly lower visual analog scale scores for pain and higher objective International Knee Documentation Committee and Tegner index scores. Radiographic evaluation showed significantly less medial joint space narrowing in the CMI group compared to partial medial meniscectomy. No significant differences between groups were reported regarding Lysholm and Yulish scores. Another long-term study compared outcomes of CMI versus partial meniscectomy in patients with concomitant ACL reconstruction. The authors concluded that patients with chronic meniscal tears treated with medial CMI reported lower levels of post-operative pain compared to meniscectomy, while acute lesions treated with CMI showed less knee laxity at follow-up (38). The CMI when performed in the acute setting showed no additional benefits when compared to partial medial meniscectomy alone (28).
Zafagnini et al. (39), in a multi-center study, evaluated the clinical outcomes of 43 patients after lateral CMI implantation. They reported improvement of all clinical scores from baseline to follow-up evaluations. At the final follow-up, 58% of the patients reported activity levels comparable to their pre-injury values, with 95% patient reported satisfaction. A higher body mass index, the presence of concomitant procedures, and a chronic injury pattern were identified as potential negative prognostic factors.
As far as concomitant open-wedge high tibial osteotomies is concerned, Gelber et al. (40) found no short-term additional benefit when compared to partial meniscectomy and meniscal scaffolding.
Final Remarks and Future Directions
The menisci are known to be heterogeneous complex structures with segmental variations according to their anatomy, biology and function. The proper understanding on the different types of meniscal injuries (both traumatic and degenerative) and their pathophysiology and pathomechanics will assist the clinician in identifying the correct indications and contraindication for each type of lesion, preserving the meniscus whenever possible. The clinical application of meniscal scaffolds is limited to CMI and Actifit. In order to successfully implant these meniscus scaffolds, it is required an intact meniscal rim and sufficient meniscal tissue at the anterior and posterior meniscus horns to attach the scaffold. When in case of axial malalignments and/or ligament insufficiencies, these must be correct prior or during the scaffold implantation. The rehabilitation protocol should be tailored to address each patient’s individual characteristics, respect the chronobiology of the scaffold tissue integration and the progression within phases should be goal-based. Novel meniscal scaffolds have been developed for addressing total meniscus reconstruction with a functional meniscus replacement, mimicking the biology and mechanical properties of the native meniscus. These novel scaffolds may further protect the articular cartilage surface of the knee joint from the extensive damage after a total meniscectomy. A second generation of implants pre-cultured in vitro allows cell adhesion and extracellular matrix production and then are implanted into the meniscal defects which will probably follow as cell seeding as has been demonstrated to improve the mechanical properties and histological results. In the future, it may be possible to improve tissue formation in the meniscal scaffold using autologous cells (e.g., stem cells) and/or growth factors (e.g., platelet-rich plasma). This strategy may augment the tissue regeneration and improve clinical results. The use of mesenchymal stem cells may also enhance a greater promotion of intrinsic meniscal healing capacity. In addition, nanotechnology and gene therapy have emerged as potential options and have showed great potential for the treatment of meniscal lesions, however its translation into the clinical setting may take a few more years. Biofabrication of patient-specific meniscal scaffolds with a 3D printer from the advanced segmentation of menisci knee MRI datasets has been showing promising results in the laboratory setting. This novel technique will allow tailoring the meniscal scaffold to the patient-specific native characteristics of the knee.
References
1. Pereira H, Cengiz IF, Silva-Correia J, Cucciarini M, Gelber PE, Espregueira-Mendes J, Oliveira JM, Reis, RL. Histology-Ultrastructure-Biology. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 23-33.
2. Halewood C, Amis AA. Physiology: Biomechanics. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 35-45.
3. Heijink A, Gomoll AH, Madry H, Drobnič M, Filardo G, Espregueira-Mendes J, van Dijk CN. Biomechanical considerations in the pathogenesis of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):423-35.
4. Ahmed A, Burke D. In-vitro of measurement of static pressure distribution in synovial joints—Part I: Tibial surface of the knee. J Biomech Eng. 1983;105(3):216-25.
5. Watanabe Y, Van Scyoc A, Tsuda E, Debski RE, Woo SL. Biomechanical function of the posterior horn of the medial meniscus: a human cadaveric study. J Orthop Sci. 2004;9(3):280-4.
6. Voloshin AS, Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomech Eng. 1983;5(2):157-61.
7. Abrams GD, Frank RM, Gupta AK, Harris JD, McCormick FM, Cole BJ. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med. 2013:0363546513495641.
8. Verdonk PC, Dhollander AA, Tampere T, Verdonk R. Meniscus Substitution: Scaffolds, Allografts and Prosthetic Implants. In: Emans PJ, Peterson L, editors. Developing Insights in Cartilage Repair. Springer; 2014. p. 253-65.
9. Verdonk R. The meniscus: past, present and future. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):145-6.
10. Di Matteo B, Tarabella V, Filardo G, Viganò A, Tomba P, Marcacci M. Thomas Annandale: the first meniscus repair. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1963-6.
11. Pereira H, Frias AM, Oliveira JM, Espregueira-Mendes J, Reis RL. Tissue engineering and regenerative medicine strategies in meniscus lesions. Arthroscopy. 2011;27(12):1706-19.
12. Cengiz IF, Pereira H, Pêgo JM, Sousa N, Espregueira‐Mendes J, Oliveira JM, Reis RL. Segmental and regional quantification of 3D cellular density of human meniscus from osteoarthritic knee. J Tissue Eng Regen Med. 2015. doi: 10.1002/term.2082.
13. Pereira H, Caridade S, Frias A, Silva-Correia J, Pereira D, Cengiz I, Mano JF, Oliveira JM, Espregueira-Mendes, J, Reis, RL. Biomechanical and cellular segmental characterization of human meniscus: building the basis for Tissue Engineering therapies. Osteoarthritis Cartilage. 2014;22(9):1271-81.
14. Cengiz IF, Pitikakis M, Cesario L, Parascandolo P, Vosilla L, Viano G, Oliveira, JM, Reis, RL. Building the Basis for Patient-Specific Meniscal Scaffolds: From Human Knee MRI to Fabrication of 3D Printed Scaffolds. Bioprinting. 2016.
15. Pereira H, Cengiz IF, Silva-Correia J, Oliveira JM, Reis RL, Espregueira-Mendes J. Human meniscus: from biology to tissue engineering strategies. In: Doral MN, Karlsson J, editos. Sports Injuries. Springer; 2015. p. 1089-102.
16. Yan L-P, Oliveira JM, Oliveira AL, Caridade SG, Mano JF, Reis RL. Macro/microporous silk fibroin scaffolds with potential for articular cartilage and meniscus tissue engineering applications. Acta Biomater. 2012;8(1):289-301.
17. Yan L-P, Silva-Correia J, Oliveira MB, Vilela C, Pereira H, Sousa RA, Mano JF, Oliveira AL, Oliveira JM, Reis, RL. Bilayered silk/silk-nanoCaP scaffolds for osteochondral tissue engineering: in vitro and in vivo assessment of biological performance. Acta Biomater. 2015;12:227-41.
18. Bacelar AH, Cengiz IF, Silva-Correia J, Sousa RA, Oliveira JM, L. RR. “Smart” Hydrogels in Tissue Engineering and Regenerative Medicine Applications. In: Khang G, editor. Handbook of Intelligent Scaffolds for Regenerative Medicine. Pan Stanford Publishing; 2015.
19. Buma P, Ramrattan N, van Tienen TG, Veth RP. Tissue engineering of the meniscus. Biomaterials. 2004;25(9):1523-32.
20. Reguzzoni M, Manelli A, Ronga M, Raspanti M, Grassi FA. Histology and ultrastructure of a tissue‐engineered collagen meniscus before and after implantation. J Biomed Mater Res B Appl Biomater. 2005;74(2):808-16.
21. Pereira H, Silva-Correia J, Oliveira J, Reis R, Espregueira-Mendes J. Future trends in the treatment of meniscus lesions: from repair to regeneration. In: Verdonk R, Espregueira-Mendes J, Monllau, JC, editors. Meniscal Transplantation. Springer; 2013. p. 103-12.
22. Stone KR, Steadman JR, Rodkey WG, Li S-T. Regeneration of Meniscal Cartilage with Use of a Collagen Scaffold. Analysis of Preliminary Data. J Bone Joint Surg Am. 1997;79(12):1770-7.
23. Verdonk R, Verdonk P, Huysse W, Forsyth R, Heinrichs E-L. Tissue ingrowth after implantation of a novel, biodegradable polyurethane scaffold for treatment of partial meniscal lesions. Am J Sports Med. 2011;39(4):774-82.
24. Van Minnen B, Van Leeuwen M, Kors G, Zuidema J, Van Kooten T, Bos R. In vivo resorption of a biodegradable polyurethane foam, based on 1, 4‐butanediisocyanate: A three‐year subcutaneous implantation study. J Biomed Mater Res A. 2008;85(4):972-82.
25. Zuidema J, van Minnen B, Span M, Hissink C, van Kooten T, Bos R. In vitro degradation of a biodegradable polyurethane foam, based on 1, 4‐butanediisocyanate: A three‐year study at physiological and elevated temperature. J Biomed Mater Res A. 2009;90(3):920-30.
26. Pujol N, Verdonk P. Actifit Polyurethane Meniscus Scaffold: Basic Science, Techniques, and Results. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 543-51.
27. Hinarejos P, Erggelet C, Monllau JC. Collagen Meniscus Implant: Basic Science, Technique and Results. In: Hulet C, Pereira H, Peretti G, Denti, M, editors. Surgery of the Meniscus. Springer; 2016. p. 531-42.
28. Rodkey WG, DeHaven KE, Montgomery WH, Baker CL, Beck CL, Hormel SE, Steadman R, Cole B, Briggs K. Comparison of the collagen meniscus implant with partial meniscectomy. J Bone Joint Surg Am. 2008;90(7):1413-26.
29. Monllau JC, Gelber PE, Abat F, Pelfort X, Abad R, Hinarejos P, et al. Outcome after partial medial meniscus substitution with the collagen meniscal implant at a minimum of 10 years’ follow-up. Arthroscopy. 2011;27(7):933-43.
30. Hirschmann M, Keller L, Hirschmann A, Schenk L, Berbig R, Lüthi U, et al. One-year clinical and MR imaging outcome after partial meniscal replacement in stabilized knees using a collagen meniscus implant. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):740-7.
31. Monllau JC. Collagen Meniscal Implant (CMI). In: Verdonk R, Espregueira-Mendes J, Monllau, JC, editors. Meniscal Transplantation. Springer; 2013. p. 73-82.
32. Implant MCM. Rehabilitation program summary for patients, surgeons, and physiotherapists. Franklin Lakes, NJ, USA: ReGen Biologics, Inc.; 2006.
33. Grassi A, Zaffagnini S, Muccioli GMM, Benzi A, Marcacci M. Clinical outcomes and complications of a collagen meniscus implant: a systematic review. Int Orthop. 2014;38(9):1945-53.
34. Zaffagnini S, Grassi A, Muccioli GMM, Bonanzinga T, Nitri M, Raggi F, Ravazzolo J, Marcacci, M. MRI evaluation of a collagen meniscus implant: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3228-37.
35. Filardo G, Andriolo L, Kon E, de Caro F, Marcacci M. Meniscal scaffolds: results and indications. A systematic literature review. Int Orthop. 2015;39(1):35-46.
36. Bulgheroni P, Bulgheroni E, Regazzola G, Mazzola C. Polyurethane scaffold for the treatment of partial meniscal tears. Clinical results with a minimum two-year follow-up. Joints. 2013;1(4):161.
37. Zaffagnini S, Muccioli GMM, Lopomo N, Bruni D, Giordano G, Ravazzolo G, et al. Prospective Long-Term Outcomes of the Medial Collagen Meniscus Implant Versus Partial Medial Meniscectomy A Minimum 10-Year Follow-Up Study. Am J Sports Med. 2011;39(5):977-85.
38. Bulgheroni E, Grassi A, Bulgheroni P, Muccioli GMM, Zaffagnini S, Marcacci M. Long-term outcomes of medial CMI implant versus partial medial meniscectomy in patients with concomitant ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3221-7.
39. Zaffagnini S, Grassi A, Muccioli GMM, Holsten D, Bulgheroni P, Monllau JC, Berbig R, Lagae K, Crespo R, Marccaci M. Two-year clinical results of lateral collagen meniscus implant: a multicenter study. Arthroscopy. 2015;31(7):1269-78.
40. Gelber PE, Isart A, Erquicia JI, Pelfort X, Tey-Pons M, Monllau JC. Partial meniscus substitution with a polyurethane scaffold does not improve outcome after an open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):334-9..
(Abstract) (Full Text HTML) (Download PDF)
Asian Journal of Arthroscopy – Vision for Tomorrow
Sachin Tapasvi, Parag Sancheti, Ashok Shyam
Volume 1 | Issue 2 | Aug – Nov 2016 | Page 1-2
Author: Sachin Tapasvi [1], Parag Sancheti [2] , Ashok Shyam [2],[3]
[1] Orthopaedic Specialty Clinic, Pune Maharashtra.
[2] Sancheti Institute for Orthopaedics & Rehabilitation, Pune, India
[3] Indian Orthopaedic Research Group, Thane, India
Address of Correspondence
Dr Ashok Shyam
AJA Editorial Office, A-203, Manthan Apts, Shreesh CHS, Hajuri Road, Thane [w], Maharashtra, India.
Email: editor@asianarthroscopy.com
The first Issue of Asian Journal of Arthroscopy was launched in Pune, India at the hands of Dr Ramchandra Tapasvi, Dr João Espregueira-Mendes, Dr David Parker, Dr Sachin Tapasvi and Dr Parag Sancheti. The first issue had a symposium on graft selection for ACL reconstruction with contributions from both international and national surgeons. We have received many positive response and also comments to improve on the format of the journal, but in the end, AJA has successfully piqued the interest of Arthroscopy Surgeons all across the globe. Surgeons have commented on the quality of the articles, on the review process and specially on indexing of the Journal. With these expectations, the responsibility of the editorial team has greatly increased to maintain the best standard for the Journal. We have identified the main areas of focus that will help AJA evolve into a truly international Journal. One of the most important aspect will be dedicated symposia on a focussed topic in each issue.
The current issue contains symposium on meniscal tears and again has contributions from various teams of surgeons. These symposiums basically reflect a combined approach of elaborating personal experiences along with literature review to provide readers with a practical and clinical article that is free of statistical aspect of the current review papers. The focus is on the surgical decision making, surgical techniques and tips and tricks of the surgery. We believe this combination provides the best reading material to practicing surgeons as well as trainees of Arthroscopy. We shall definitely continue this tradition of dedicated symposia in future. The forthcoming symposium is on shoulder instability and Dr Jonathan Herald from Sydney Australia will be the guest editor for the issue. The second focus area is collecting surgical videos and techniques. Arthroscopy is a branch which is much more visual than theoretic and videos are the best form of visual aid that an academic journal can provide. We will be creating a separate section which will look after this aspect of video articles and we invite our readers to submit their surgical videos for publication in AJA. The third area is peer review, which is the main academic backbone of any journal. AJA has a policy of blinded peer review and every article will be sent for peer review to at least three reviewers. This may take some time, as we have less number of reviewers currently, but we request our authors to be a bit patient with us. We will also request all our authors and readers to join us a reviewers also. They can do so easily by creating an account in ‘scripture’ and adding reviewer to the profile. The review process will be exclusively through the online journal system and all records will be saved for future references. We also offer our reviewers a certificate for reviewing articles and publish their names in the first issue of every year. The last focus area is indexing of the Journal, which we are trying to push aggressively. The journal has received the ISSN number and copy of the first issue has been submitted to various indexing bodies. However we know that all indexing bodies will take time for assessment of the journal and real Indexing and assessment of journal will only be at the end of successful two years of the Journal. The steps toward fulfilling all criteria’s for major indexes are actively taken from the first issue itself. The editorial board of AJA firmly believes in the idea and concept of AJA and we the support of our readers, authors, and reviewers we believe we can make AJA the very best in the world.
Dr Sachin Tapsvi | Dr Parag Sancheti | Dr Ashok Shyam
Dr. Sachin Tapasvi
Dr. Parag Sancheti
Dr. Ashok Shyam
(Abstract) (Full Text HTML) (Download PDF)
Asian Journal of Arthroscopy – Insights
Sachin Tapasvi, Parag Sancheti, Ashok Shyam
Volume 1 | Issue 1 | April – Jun 2016 | Page 1-2
Author: Sachin Tapasvi [1], Parag Sancheti [2] , Ashok Shyam [2],[3]
[1] Orthopaedic Specialty Clinic, Pune Maharashtra.
[2] Sancheti Institute for Orthopaedics & Rehabilitation, Pune, India
[3] Indian Orthopaedic Research Group, Thane, India
Address of Correspondence
Dr Ashok Shyam
AJA Editorial Office, A-203, Manthan Apts, Shreesh CHS, Hajuri Road, Thane [w], Maharashtra, India.
Email: editor@asianarthroscopy.com
“Technique, Technique, Technique”, although Dr David Hungerford quoted the above for arthroplasty surgery, the same applies to Arthroscopy. Surgical technique and skill are unique to Arthroscopy almost as if it is a distinct area of expertise. No other subspecialty of orthopaedics has such minimal overlap with general orthopaedics, in terms of surgical techniques. One of the major goals of Asian Journal of Arthroscopy (AJA) is propagation of arthroscopy techniques. ‘Training by Publication’ is one the founding pillars of AJA. We want to bring the best techniques and procedures to our readers. These techniques will be in form of articles, pictograms and videos with basic premise of ease of learning. The readers should be able to understand the principles of the surgery, the critical steps and also learn new tips and tricks. They should be able to execute steps on the surgery and possibly embark on the learning curve to master the technique. Although more work is needed in terms of envisioning the formats of the article, this remains the mail goal of AJA and in times to come we would look for ways and means to do this more effectively. Currently the Journal has a technical note/video technique section with guidelines to submit a video article. We will also be running pictograms or Photo-articles which will be more pictures and less text (something like a comic strip but with much more smiles for arthroscopy surgeons!). ArthroMedia is a special section on the AJA website which will host multiple media items like videos, powerpoints, PDF and other documents related to surgical skills and surgeries. This will be compiled from contributions of editorial board, reviewers board, authors and also from our readers. This section will be open for submission to all and will compile the best training content. We invite all of you to submit your content to ArthoMedia and help us build this portal.
Why the new Journal when there are already existing journals of Arthroscopy?
There are two main reasons; to produce a body of literature that is clinically relevant and to make this knowledge freely accessible to all. Journals have shown trend to move towards a more rigid framework of scientific publications, meanwhile losing the mail focus of scientific publications. Journals are meant to directly influence and improve patient care. Charging for downloading articles imposes another limitation on dispersion and use of knowledge. AJA intends to counter these two issues by creating a journal that is intelligent, interactive, and clinically relevant and at the same time completely Open Access. The entire format of the Journal will be one of ‘Integration’ with basic science, molecular research, clinical trials, clinical research, case based discussion, evidence based medicine, expert opinion and patients perspective, all aiming together to ‘Translate’ into betterment of Arthroscopy strategies and surgeries. Although the Journal will focus on Asian studies, it will be open to submissions from all across the globe.
The Journal will be open access, peer reviewed and will have three issues every year. It will be published in both online and print formats. The Journal is the official Arthroscopy Journal of the Orthopaedic Research Group. The Research Group has affiliation to Ebscohost and is a member of Crossref. Thus primarily the journal will be indexed with Ebscohost and will have a doi (digital object identifier) for each article. Within due course we aim to index the journal with all major indexes including Pubmed and Science citation index.
What is unique about AJA?
The most important unique point of AJA is that it is a Surgeon Initiated Journal. The entire concept of the journal, the designing of website, manuscript portal and guidelines are all made by a team of surgeons. The team will be self-publishing the Journal and there will be no external publisher involved. All the rights of the journal is with the editorial board and the core team of AJA and no rights belong to any external body. This gives us a lot of flexibility and helps the journal to adapt rapidly to changing needs of the readers and authors. The journal decisions can be taken rapidly and since the entire process is controlled by the AJA team, the quality of peer review and content will be excellent. With no constraint of a corporate publisher, we can lay down our own rules and regulations and provide best of services to the Arthroscopy community
We believe AJA is an ambitious project and has much potential to evolve along with the evolution of Arthroscopy Surgery. We have great plans for AJA and we hope for great co-operation from the Arthroscopy community. Please do send your suggestions, opinions and comments to us at the editorial email. AJA is a journal “By the Surgeon, for the Surgeon, and of the Surgeon” and together we can take it to great heights
Dr Sachin Tapsvi | Dr Parag Sancheti | Dr Ashok Shyam
Dr. Sachin Tapasvi
Dr. Parag Sancheti
Dr. Ashok Shyam
(Abstract) (Full Text HTML) (Download PDF)
Arthroscopic reduction and Internal fixation (ARIF) using Parapatellar Approach – A modality for treating fracture Tibial eminence with ACL injury.
Vikram V Kadu, K A Saindane, Ninad Goghate, Neha N Godghate
Volume 1 | Issue 1 | April – Jun 2016 | Page 43-45
Author: Vikram V Kadu [1], K A Saindane [1], Ninad Goghate [1], Neha N Godghate [1]
[1] ACPM Medical College, Dhule – 424001, Maharashtra, India
Address of Correspondence
Dr. Vikram V. Kadu
ACPM Medical College, Dhule – 424001, Maharashtra India
Email : vikram1065@gmail.com
Abstract
Introduction:Arthroscopic reduction and internal fixation (ARIF) of tibial intercondylar eminence fractures is the emerging state-of-the-art. Tibial eminence fractures underwent arthroscopic evaluation when closed reduction after aspiration failed to yield an anatomic reduction. Arthroscopic reduction and fixation of avulsion fractures of the tibial eminence restores the length of the ACL, provides stable fixation promoting early motion.
Materials and Methods: This is a retrospective study conducted between 2010 and 2012. All 40 patients suffering ACL injury with tibial eminence fracture were stabilized in the emergency room followed by above knee slab. Once the patient was stabilized surgery (Arthroscopic reduction and internal fixation) was performed. The technique involved arthroscopic placement of a 3.5-mm cannulated compression screw into the tibial eminence. Patients were placed in a standard postoperative ACL protocol. Assessment was done using knee society score.
Result: All fractures demonstrated radiographic healing by 8 weeks, and none of the patients had subjective complaints of pain and instability. At 2 yrs follow-up all the patients had functional range of motion (00-1600) and returned successfully to their previous work. In our series we didn’t come across any complication.
Conclusion: Arthroscopic reduction and screw fixation with a cannulated screw is a simple, effective, and safe technique providing stable fracture fixation to allow immediate mobilization with minimal loss of extension.
Key words : ACL avulsion fracture, Arthroscopic, cannulated screw
Introduction
The intercondylar eminence serves as the point of attachment for portions of the menisci and the anterior and posterior cruciate ligaments(1). In addition to disrupting ACL continuity, intercondylar eminence avulsion fractures, depending on size, may affect weight-bearing aspects of the articular surface of the tibia.
Fracture of the tibial intercondylar eminence is a consequence of ACL avulsion at its insertion(2). Mechanism being same as of ACL rupture it is pulled from the tibia with a piece of the bony plateau. These injuries are commonly related to high energy trauma usually road traffic accidents and have high incidence of associated injuries.
Fractures of the tibial intercondylar eminence were classified into 3 types3: type I, minimal or nondisplaced; type II, partially displaced or hinged fracture; and type III, completely displaced. Surgical treatment is currently recommended for type II and III displaced fractures. Open methods were conventionally used to fix these avulsions however now arthroscopic treatment is the standard of care. Most of the existing literature is from the western world and publications from India are very few. We present our series of arthroscopic fixation done for ACL avulsion fracture performed at a district level rural center in India
Materials and Methods:
This is a retrospective study conducted on 40 patients suffering ACL injury with tibial eminence fracture between 2010 and 2012. Patients were stabilized in the emergency room followed by above knee slab. Of the 40 patients 27 were male and 13 female. 26 were right sided and 14 left sided. 28 suffered RTA and 12 had fall. Mean age of the patient was 35 yrs (range 23 – 47 yrs). After stabilizing the patient, surgery (Arthroscopic reduction and internal fixation with 3.5 mm screw) was performed. The technique involved arthroscopic placement of a 3.5-mm cannulated compression screw into the tibial eminence. Patients were placed in a standard postoperative ACL protocol. All patients were clinically and radiographically reviewed for 2 years and assessed with knee society score.
Surgical Technique:
In supine position with the knee flexed 70° to 90°. Pneumatic tourniquet was used. Standard knee arthroscopy was performed with anterolateral and anteromedial portals. In all patients, an additional antero-superior parapatellar portal was used for wider and better view of the intercondylar tibial eminence.
Figure 1: showing the entry portals.
Through the standard anteromedial portals, using Normal saline under gravity the hemarthrosis was washed out using the shaver, the hematomas at the fracture site were debrided, and the joint was inspected for the presence of any other intra-articular lesions. Turning the optics anteriorly, the intermeniscal ligament was identified, and in cases with interposition, the ligament was shifted aside using a probe introduced through the standard anteromedial portal to make reduction possible. Sometimes the ligament needs to be partially cut. After the anatomic condition and integrity of the ACL were carefully confirmed, the probe was then used via the anteromedial portal to reduce the fracture in its bony bed.
Under arthroscopic vision, the midpoint of the inferior non-articular surface of the patella is selected and a guide wire of 1.2 mm was then passed perpendicular to this surface, in the direction of the center of the fracture site with the knee flexed to approximately 70° to 90°. The portal was then drilled using a 2.7 mm cannulated drill bit and fragment was fixed with 3.5 mm cannulated screw.
Case: 30 yrs old male labourer by occupation suffered an RTA and presented with complaints of pain and swelling over left knee joint and restriction of movements. Clinically the patient had instability at the knee joint. X-rays both AP and Lateral view were taken (Fig 2A) which showed fracture tibial eminence. The patient was given above knee slab and was admitted. Surgery (Arthroscopic reduction and internal fixation with 3.5 mm screw) was performed. Post- operatively the patient was given long leg knee brace. Physiotherapy in the form of Quadriceps exercises was started immediately and knee bending (upto 30 degrees) and partial toe touch bearing walking with walker with long leg knee race on post-op day 2 once the drain was removed. Patient was followed up after 1 month (Fig 2B). X ray showed uniting fracture. Knee bending was increased from 30-60 degrees and 50 % weight bearing allowed. At 2 months (Fig 2C) X ray showed radiological union and patient was advised full weight bearing walking with walker and brace, knee ROM exercises were started and complete flexion and extension was allowed. At 12 weeks (Fig 2D). X rays at 10 months follow-up (Fig 2E). At 2 yrs and 7 months follow up (Fig 2F). The patient has full range of motion (0-160o) (Fig 2G &H) and returned to his previous work.
Figure 2A: pre-op AP and LAT view
Figure 2B: Radiograph at 1 month follow-up
Figure 2C: Radiograph at 2 months follow-up
Figure 2D: Radiograph at 3 months follow-up
Figure 2E: Radiograph at 10 months follow-up
Figure 2F: Radiograph at 2yrs and 7 months follow-up
Figure 2G: Radiograph at 10 months follow-up
Figure 2H: Radiograph at 10 months follow-up
Observations and Results:
All the 40 patients were assessed at the end of 2 yrs and we found out that, all patients had functional range of movement of the knee joint and they returned to their previous work. There was no evidence of any infection or complication in our study. There was no failure of fixation and no other complications in our series
Discussion:
Tibial spine fractures usually result from a twisting movement of the knee. Abnormal valgus/varus or hyperflexion /hyperextension forces can cause avulsion of the tibial eminence. Such injuries are common after road traffic accidents or sporting activities.
Arthroscopic reduction internal fixation of intercondylar eminence avulsion is recommended for all displaced type III fractures and should be considered in all cases of displaced type II fractures. Various studies by different authors have been reported for these kind of fractures(2,4-10). Tibia eminence fracture results in anterior knee instability and occasionally anterior impingement during knee extension when the avulsion fragment is displaced(11). The goal of treatment for displaced tibial intercondylar eminence fracture is anatomic reduction. Disadvantages of screw fixation include risks of comminution of the fracture fragment, impingement due to prominent screw head, and the need for hardware removal. Because of these risks, some surgeons preferred arthroscopic reduction and internal fixation using non-absorbable sutures passed through drill holes. Suture techniques may obviate the need for a second surgery for implant removal and impingement; but arthrofibrosis and limitation of joint motion due to postoperative immobilization have been reported(2.) It has been found that antegrade screw fixation is more effective in obtaining initial rigid fixation than pull-out suture fixation for ACL avulsion fractures(12).
Tibial eminence fractures have excellent prognosis. Previously, prolonged immobilization may lead to arthrofibrosis and a permanent loss of full extension. Therefore, earlier rehabilitation is crucial as it encourages a faster recovery and prevents the development of secondary complications. Rehabilitation is similar to ACL tear protocols activities include static cycling, leg presses, elastic theraband or tubing exercises.
The technique described in this report not only helps achieve good interfragmentary compression, but also prevents undue prominence of the screw head owing to its proper direction. The bicortical purchase of the screw adds to the stability of fracture fixation, allowing early joint movement and weight bearing. The parapatellar portal secures good visualization of the operative field, enabling the screw to fix the fracture fragment perpendicularly. Although rare but chances of fracture in cases of poor bone quality is to be considered.
Conclusion
Arthroscopic reduction and internal fixation with cannulated screws for type 3B fractures having ACL injury is a novel method with good results and without any complications.
References
1. Wiss DA, Watson JT. Fractures of the tibial plateau. In:Rockwood CA, Green DP, Bucholz RW, Heckman JD, eds. Rockwood and Green’s fractures in adults.Philadelphia: Lippincott-Raven, 1996;1920-1953.
2. Berg EE. Comminuted tibial eminence anterior cruciate ligament avulsion fractures: Failure of arthroscopic treatment. Arthroscopy1993;9:446-450.
3. Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1970; 52(8):1677-1684.
4. McLennan JG. The role of arthroscopic surgery in the treatment of fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Br1982;64:477-480.
5. Falstie-Jensen S, Sondergard Petersen PE. Incarceration of the meniscus in fractures of the intercondylar eminence of the tibia in children. Injury1984;15:236-238.
6. Matthews DE, Geissler WB. Arthroscopic suture fixation of displaced tibial eminence fractures.Arthroscopy1994;10:418-423.
7. Osti L, Merlo F, Bocchi L. Our experience in the arthroscopic treatment of fracture-avulsion of the tibial spine. Chir Organi Mov1997;82:295-299.
8. Kocher MS, Micheli LJ, Gerbino P, Hresko MT. Tibial eminence fractures in children: Prevalence of meniscal entrapment.Am J Sports Med2003;31:404-407.
9. Chandler JT, Miller TM: Tibial eminence fracture with meniscal entrapment.Arthroscopy1995;11:499-502.
10. Berg EE. Comminuted tibial eminence anterior cruciate ligament avulsion fractures: Failure of arthroscopic treatment. Arthroscopy1993;9:446-450.
11. Senekovic V, Veselko M. Anterograde arthroscopic fixation of avulsion fractures of the tibial eminence with a cannulated screw: Five-year results.Arthroscopy2003;19:54-61.
12. Kendall NS, Hsu SY, Chan KM. Fracture of the tibial spine in adults and children. A review of 31 cases. J Bone Joint Surg Br. 1992; 74(6):848-852.
13. Berg EE. Comminuted tibial eminence anterior cruciate ligament avulsion fractures: failure of arthroscopic treatment.Arthroscopy. 1993; 9(4):446-450.
14. Tsukada H, Ishibashi Y, Tsuda E, Hiraga Y, Toh S. A biomechanical comparison of repair techniques for anterior cruciate ligament tibial avulsion fracture under cyclic loading. Arthroscopy. 2005; 21(10):1197-1201.
Dr. Vikram V. Kadu
Dr. K. A. Saindane
Dr. Ninad Godghate
Dr. Neha N Godghate
(Abstract) (Full Text HTML) (Download PDF)
Arthroscopic Biopsy and MRI Diagnosis in Monoarticular Joint Synovitis of Undifferentiated Origin – A retrospective study in 34 cases
Sundararajan S R, Jain Sachin Ramesh, S Rajasekaran
Volume 1 | Issue 1 | April – Jun 2016 | Page 38-42
Author: Sundararajan S R [1], Jain Sachin Ramesh [1], S Rajasekaran [1]
[1] Ganga Hospital, 313, MTP road, Coimbatore , Tamilnadu, India Pin code – 641043
Address of Correspondence
Dr Sundararajan S R
Ganga hospital, 313, MTP road, Coimbatore , Tamilnadu, India,
Pin code – 641043
Email id – sundarbone70@hotmail.com
Abstract
Purpose: The main purpose of the study was to evaluate arthroscopic biopsy results and MRI findings in monoarticular joint synovitis with emphasis on differentiation between tuberculosis and rheumatoid cases using MRI features by Choi et al.
Materials and methods: Between 2010 and 2014, 34 patients were retrospectively analyzed from our database. Clinical history, MRI findings, arthroscopy findings & biopsy reports were evaluated. Findings of Choi et al was used to correlate MRI and biopsy results between rheumatoid and tuberculosis cases. Ability of MRI in diagnosing other cases like PVNS, hemangioma was also evaluated. Samples obtained from biopsy were sent to two laboratories in 23 of our cases where MRI was suggestive of infective or inflammatory etiology.
Results: Out of 34, 9(26.47%) cases were of chronic nonspecific synovitis, 7(20.58%) cases of tuberculous synovitis, 7(20.58%) cases of rheumatoid synovitis, 3(8.8%) cases of PVNS, 2(5.88%) cases of Synovial hemangioma, and 6 others. Out of 34, tissue biopsy diagnosis was made in 25(73.53%) and MRI diagnosis was obtained in 22/34 (65%) of our patients. Using features described by Choi et al, 100% of tuberculosis cases and 57.14% of rheumatoid cases were diagnosed on MRI. A mismatch of 4/23(17.4%) was found between the reports from two recognized labs.
Conclusions: Arthroscopic biopsy and MRI are reliable techniques, with better success rate in the diagnosis of monoarticular synovitis of unknown etiology. Choi et al’s MRI recommendations are reliable in differentiating between infective or inflammatory etiology.
Keywords: Synovitis, Monoarticular, Undifferentiated, arthroscopic biospy
Introduction
Monoarticular joint synovitis of undifferentiated etiology (1), presents with complaints of pain and swelling which is not responding to anti-inflammatory treatment. Diagnosis and approach to treatment in such cases is very important for satisfactory clinical results. Arthroscopy is the preferred mode for biopsy (2-7) and provides macroscopic evaluation(3,8,9) of the monoarticular joint disease. Early diagnosis of tubercular synovitis is important to prevent joint damage(7) within few days to weeks. Similarly, inflammatory synovitis like rheumatoid synovitis also carries a prognostic significance if diagnosed early and treated(8).
Plain radiograph in early synovial disease usually remains normal for at least 6 to 12 months after symptom onset(10). MRI is a highly sensitive tool to evaluate early undifferentiated synovitis and guide the management plan(11,12). It gives the extent of synovial hypertrophy(12) with sites of increased activity with gadolinium enhancement for directing biopsy(12,13). MRI features described by Choi et al(14), where they considered synovial thickening, bone erosions, rim enhancement at bone erosions, soft tissue edema and extraarticular cystic masses for differentiating tubercular and rheumatoid synovitis.
Our hypothesis is that MRI can diagnose the specific etiology, especially the tubercular and rheumatoid synovitis, in monoarticular joint synovitis of undifferentiated origin using the MRI features described by Choi et al (14).
Methods
The study was approved by ethics committee of our institution. Between 2010 and 2014, 34 patients were retrospectively analyzed from our database using the inclusion and exclusion criteria (Flowchart 1). Clinical history, MRI findings, arthroscopy findings and biopsy reports were evaluated. Blood investigation like Rheumatoid factor, anti cyclic citrullinated protein (CCP) was used to diagnose inflammatory arthritis like rheumatoid and those cases were excluded from our study. If a patient presenting to our center for the first time without any waiting period then our policy is to give 2 weeks of anti-inflammatory medications and if symptoms don’t subside than we go ahead with other investigation of MRI, blood tests and immediate arthroscopic biopsy depending on MRI reports. If patient has already has waited for more than 2 weeks then we directly investigate with MRI, blood tests and go ahead with arthroscopic treatment.
Flowchart 1: Total no of cases included with inclusion and exclusion criteria in the study
Out of 34 joints, 26 knees, 5 ankles, 2 hips and 1 shoulder joint were included. Out of 34 patients 22 were males and 12 females between ages 9 years and 70 years. According to Choi et al(14) as described in table 1, if uniform synovial thickening, large size of bone erosion, and extra articular cystic masses more frequent and more numerous, then tubercular synovitis(14) and if more the degree of synovial hypertrophy without associated findings were present then diagnosis of rheumatoid synovitis(14) was considered. We used these findings to correlate MRI and biopsy results retrospectively between rheumatoid and tuberculosis cases.
Table 1: Criteria and grading on MRI based on Choi et al (14) to differentiate between rheumatoid and tubercular synovitis
Arthroscopic evaluation was performed by a single senior arthroscopy consultant of our institution. On arthroscopic evaluation, joint was thoroughly inspected through standard portals. Macroscopic evaluation of the joint done and the suspected area of increased activity were chosen for biopsy. At least 6 different sites in the joint was considered for biopsy, material was packed in formalin filled glass bottle and sent for histopathological examination. Arthroscopic partial or subtotal synovectomy was done if needed. Biopsy samples were sent to two different laboratories only when MRI diagnosis showed chronic synovitis of infective or inflammatory etiology, where the cause was doubtful. To be sure of the diagnosis, biopsy material was sent in these patients by two experienced senior pathologist. . Depending upon the biopsy results further treatment was initiated. No prophylactic anti-tubercular treatment was started as biopsy results usually arrived in a week for definitive treatment. Arthroscopic biopsy samples were sent to two labs for evaluation only where diagnosis of inflammatory or infective origin was doubtful on MRI in 23 out of 34 cases
Results
In our case series, Out of 34, 9(26.47%) cases were of chronic nonspecific synovitis, 7(20.58%) cases of tuberculous synovitis, 7(20.58%) cases of rheumatoid synovitis, 3(8.8%) cases of PVNS, 2(5.88%) cases of Synovial hemangioma, and 6 others. Out of 34, tissue biopsy diagnosis was made in 25(73.53%) and MRI diagnosis was obtained in 22/34 (65%) of our patients. Using features described by Choi et al, 100% of tuberculosis cases and 57.14% of rheumatoid cases were diagnosed on MRI (Table 1). There was a mismatch in biopsy results among 4 (17.4%) out of the 23 cases that were sent to two recognized laboratories simultaneously.
Discussion
Monoarticular synovitis of unexplained origin (5) needs a series of tests like blood investigation, MRI and biopsy to find out the causal factor. Effectiveness of arthroscopic biopsy in the diagnosis of monoarticular synovitis was discussed (4,6,17) earlier. We attempted to determine the same in this series along with effectiveness of MRI diagnosis. Conditions like synovial hemangioma and PVNS is done quite accurately (19,20,21) using MRI, but there is difficulty in diagnosing or differentiating infective versus inflammatory etiology. Choi et al(14) was the first to evaluate and differentiate these two conditions using MRI. We evaluated the suggested guidelines in this study.
Arthroscopy plays an important role in diagnosis(2,4,15). Major use is in the patients presenting with unexplained knee pain whose symptoms are disproportionate to the radiologic features or refractory to standard course of medical treatment(2). Arthroscopic synovial biopsy is considered as the ‘gold standard'(16) for biopsy in monoarticular joint synovitis. Arthroscopy is an excellent tool to visualize the synovium macroscopically(3,8,9), evaluate the villi precisely and obtain biopsy from site correlating with clinical findings for microscopic evaluation3,6,8. Macroscopic evaluation of normal synovium looks bland and devoid of villi, granularity or increased vascularity(8).
Figure 1a: Arthroscopic view of knee joint through anterolateral portal showing synovial hypertrophy (small arrows) in the suprapatellar fossa with 30 degree lens and camera facing 4 ‘o clock position.
Figure 1b: MRI showing extensive bony edema(26.90mm), synovial hypertrophy(11.78mm), multiple bony erosions(14.44mm), and extra articular cystic masses(*) favoring diagnosis of tuberculous synovitis.
Figure 1c: Histopathology findings showing epitheloid cells and granulomatous inflammation (arrow) suggestive of tuberculosis.
Arthroscopic findings can alter or add to the treatment plan which includes surgical tissue resection or medical treatment like Disease Modifying Anti-rheumatic Drugs (DMRD’s) to the current treatment(2). Goeb et al(22) suggested that early diagnosis and early treatment initiation in patients with inflammatory arthritis can be possible by precise arthroscopic biopsy sample from the most representative pathological areas. Chen et al(14) evaluated the role of arthroscopy in unilateral knee arthritis where they accurately diagnosed 71 cases and 3 cases were undiagnosable(4). They reported 39/74 (52.9%) cases as rheumatoid arthritis4. In our study, despite thorough arthroscopic and microscopic evaluation, we were not able to accurately diagnose in 26.47% of the patients, which were finally diagnosed as chronic non specific synovitis. Chronic non specific synovitis is also known as monoarthritis of unknown origin (5), 80% of these can go into complete remission over a period of two years(5) with just conservative treatment.
Figure 2a: Arthroscopic view of knee joint through anterolateral portalshowing reddish brown tumor with telangiectatic arterioles suggestive of hemangioma(H) in the lateral aspect of suprapatellar fossa with 30 degree lens and camera facing 12 ‘o clock position.
Figure 2b: Arthroscopic biopsy done through the anterolateral portal from multiple sites with basket punch. Note bleeding from the tumor site (arrow).
As definitive treatment with antitubercular medication is available, diagnosis of early tuberculous synovitis is very essential to prevent cartilage damage. Arthroscopic definitive tissue diagnosis and timely treatment helps in achieving excellent results in 3 – 4 months period (7), with complete symptomatic relief and full joint function restoration(7). Early rheumatoid arthritis carries a prognostic value as disease modifying agents can be introduced, which can reduce the aggressiveness of the disease by inhibiting the progressive structural damage (8). In inflammatory synovitis like early rheumatoid arthritis complete remission or marked improvement is seen in most of the patients(11,15,18).
Out of 34 cases, 23 cases had synovial hypertrophy arthroscopically for which partial or subtotal synovectomy was performed to aid in clinical remission. In case of pigmented villonodular synovitis and synovial hemangioma, MRI guides the diagnosis in all the patients following which arthroscopic extended synovectomy and arthroscopic excision is the preferred treatment(19,20,21) which was performed in our 4 cases.
MRI is a highly sensitive tool for evaluation of patients presenting with undifferentiated synovitis(1). It can detect bony edema, cartilage erosions also when combined with gadolinium enhancement, degree of synovial thickening (pannus) and intraarticular lesions can be picked up (1). In MRI, to differentiate between infective or inflammatory etiology is very difficult. But the extent of synovial hypertrophy, articular cartilage damage and other findings like cartilaginous loose bodies which are not visible on plain radiograph can be detected. Treatment plan can be based upon MRI to guide the site for arthroscopic biopsy, to have a baseline value of synovial hypertrophy if there is recurrence after synovectomy. MRI diagnosis in cases like synovial hemangioma and Pigmented villonodular synovitis (PVNS)(19,20,21) is accurate, as observed in this study too, where extended synovectomy can be planned preoperatively to avoid recurrence. However in a case report by Lee et al (23), where MRI suggested a diagnosis of Pigmented villonodular synovitis due to the hemosiderin deposits and a nodular mass around the knee joint but biopsy revealed it to be tuberculosis. They suggested that the first step in diagnosis of tuberculous knee arthritis is to have high index of suspicion (23). So, even biopsy remains the main means of diagnosis even in such cases.
Figure 2c: Piecemeal excision (arrow heads) of the tumor done with arthroscopic scissors through the anterolateral portal with 30 degree lens and camera facing 12′ o clock position.
Figure 3a: MRI of right shoulder showing synovial hypertrophy (18.33mm) with rice bodies (arrow).
Figure 3b: Histopathology after arthroscopic biopsy of the same shoulder, showing synoviothelial hyperplasia (arrow). Perivascular aggregates of plasma cells with russel bodies (circled) suggestive of rheumatoid synovitis
Overall, MRI agreed with biopsy in 22/34 (65%) of our patients. On using MRI features for finding rheumatoid and tuberculous synovitis, tuberculosis was diagnosed in 7/7(100%) and rheumatoid in 4/7(57.14%) of the cases (Table 2).
Table 2: Arthroscopic biopsy results and its correlation with MRI
Gadolinium enhancement was used in 3 (2 cases were rheumatoid and 1 case was tuberculosis) out of 14 of our patients with tuberculosis and rheumatoid. Enhancement of bone and synovium and also the rim enhancement was similar in both the scenarios. This led us look for other factors in these cases to differentiate between them. Lymph nodes were enlarged in tuberculosis as compared to none in rheumatoid. Also the erosions were multiple and large in tuberculosis as compared to rheumatoid cases. Overall, it was the combination of extensive synovial hypertrophy, multiple large bony erosions, extensive edema, extraarticular mass and enlarged lymph nodes which favored the diagnosis of tuberculosis. Also, synovial hypertrophy with minimal erosion, mild to moderate edema, with no extraarticular masses and no enlarged lymph nodes favored the diagnosis of rheumatoid. Further evaluation for the need of gadolinium contrast agent is needed to assess its real use in differentiating these two conditions.
Arthroscopic biopsy samples were sent to two labs for evaluation in 23 out of 34 cases. Out of which 20 reports matched each other. There was disagreement in 4 out of 23 (17.4%) cases. Out of 4 cases, 3 cases were reported by the lab as chronic non specific synovitis and 1 case of suppurative synovitis which was diagnosed by other lab as 3 cases of rheumatoid and 1 case of tuberculous synovitis, respectively. Implications of correct diagnosis are well known, especially in the case of tuberculosis where there is specific treatment available and complete remission is possible, if it is missed, complete destruction of the joint is inevitable. Therefore it is important to send biopsy samples to at least two laboratories that can increase the probability of correct diagnosis in patients.
Limitation of the study
Several limitations must be taken into consideration in this study. Firstly, the sample size of our study group is small and multiple joints were included, because of the rarity in monoarticular synovitis cases in general, but still it is better than most of the other studies. Secondly, analysis of the MRI was done by single experienced radiologist at our institution. So, effects of interobserver variability could not be assessed in this study. Thirdly, gadolinium enhancement was not performed on every case as we were in initial stages to give enhancement to monoarticular joint synovitis cases before this study was considered, so Choi et al.’s criteria couldn’t be replicated to the exact similarity. Finally, only 23 cases (out of 34) were sent to two laboratories, further reducing the sample size, because of the institute policy to send them to two labs only where diagnosis of inflammatory or infective origin was doubtful on MRI.
Conclusion
Arthroscopic biopsy and MRI both are reliable techniques, with better success rate in the diagnosis of monoarticular synovitis of unknown etiology. Choi et al’s MRI recommendations may aid in differentiating between infective or inflammatory etiology of monoarticular joint synovitis.
References
1. Yasser E, Yasser R. The diagnostic dilemma of undifferentiated inflammatory synovitis of the knee joint/joints: a comprehensive approach. APLAR Journal of Rheumatology 2007 Sep; 10(3):182–189
2. O’Rourke KS, Ike RW. Diagnostic arthroscopy in arthritis patient. Rheum Dis Clin North Am. 1994 May; 20(2):321-42
3. Kurosaka M, Ohno O, Hirohata K. Arthroscopic evaluation of synovitis in the knee joints. Arthroscopy. 1991; 7(2):162-70
4. Chen GQ, Zhang HW, Li ZF,Guo DM, Yu YT. Significance of arthroscopy in the diagnosis of unilateral knee arthritis. Zhonghua Yi Xue Za Zhi. 2010 Jun15; 90(23):1615-7.
5. Scherer T, Kieser C, Gerber H. Assessment and course of 110 patients with monoarthritis. Ther Umsch. 1989 Apr; 46(4):258-64
6. Schulte E, Fisseler-Eckhoff A, Muller KM. Differential diagnosis of synovitis. Correlation of arthroscopic-biopsy to clinical findings. Pathologe. 1994 Feb; 15(1):22-7
7. Cai D, Chen Y, Rong L. Arthroscopy in diagnosis and treatment of tuberculous synovitis. Zhonghua Jie He He Hu Xi Za Zhi. 1998 May; 21(5):276-7
8. Mihir D Wechalekar, Malcolm D Smith. Utility of arthroscopic guided synovial biopsy in understanding synovial tissue pathology in health and disease states. World J orthop 2014 Nov;5(5):566-573
9. Masahiro K, Osamu O, Kazushi H. Arthroscopic evaluation of synovitis in knee joints. Arthroscopy. 1991;7(2):162-170
10. Van der Heijde DM. Plain X-rays in rheumatoid arthritis: overview of scoring methods, their reliability and applicability. Baillieres Clin Rheumatol. 1996 Aug;10(3):435-53
11. M ostergaard, B Ejbjerg, M Stoltenberg et al. Quantitative magnetic resonance imaging as marker of synovial membrane regeneration and recurrence of synovitis after arthroscopic knee joint synovectomy: a one year follow up study. Ann Rheum Dis 2001;60:233-236
12. F.M.McQueen. Magnetic resonance imaging in early inflammatory arthritis: what is its role? Rheumatology 2000;39:700-706
13. Matthew A., Doris E., Mark A. MR imaging of synovial disorders of the knee: An update. Radiologic Clinics Of North America 2007;45:1017-1031
14. Jung-Ah Choi, Sung Hye Koh et al. Rheumatoid arthritis and tuberculous arthritis: Differentiating MRI features. American Journal of Roentgenology 2009 Nov;193(5):1347-1353
15. GAO Jun, GAO Chun-Sheng, GAOYa-zhou et al. Clinical study on arthroscopic examination in diagnosis and treatment of knee synovitis. Journal of clinical and experimental medicine 2013-09
16. Smith MD, Baeten D et al. Standardisation of synovial tissue infilterate analysis: how far we have come? How much further do we need to go? Ann Rheum Dis 2006;65:93-100
17. Onis Singhal, Viplesh kaur et al. Arthroscopic synovial biopsy in definitive diagnosis of joint diseases: An evaluation of efficacy and precision. International Journal of applied and basic medical research, 2012 Jul-Dec;2(2)
18. Ayral X, Bonvarlet JP et al. Arthroscopy-assisted synovectomy in the treatment of chronic synovitis of the knee. Revue du Rhumatisme, 1997,64(4):215-226
19. Rochwerger A, Groulier P et al. Pigmented villonodular synovitis of the knee. Treatment results in 22 cases. Revue de Chirurgie Orthopedique et Reparatrice de L’appareil Moteur, 1998; 84(7):600-606
20. Alessandro De Ponti, Valerio Sansone et al. Result of arthroscopic treatment of Pigmented villonodular synovitis of the knee. Arthroscopy, 2003 Jul-Aug;19(6):602-607
21. Jeung-Tak Suh, Sang-Jin Cheon, Sung-Jong Choi. Arthroscopy, 2003 Sep,19(7):e77-e80
22. Goeb V, Walsh CA, Reece RJ, et al. Potential role of arthroscopy in the management of inflammatory arthritis. Clin Exp Rheumatol, May-June 2012, 30(3) p429-35
23. Lee DH, Lee DK, Lee SH, et al. Tuberculous arthritis of knee joint mimicking pigmented villonodular synovitis. Knee Surg Sports Traumatol Arthrosc, May 2012, 20(5) p937-40
Dr. Sundararajan S R
Dr. Sachin Jain
Dr. S Rajasekaran
(Abstract) (Full Text HTML) (Download PDF)